Abstract
INTRODUCTION
The elderly are often underrepresented in clinical trials for acute coronary syndrome (ACS), and cardiologists commonly face management dilemmas in the choice of treatment for this group of patients, particularly concerning the use of invasive revascularisation. This study analysed the characteristics of hospitalised elderly patients with ACS, and compared the outcomes of treatments.
METHODS
From 29 December 2005 to 26 April 2010, 13,545 patients were admitted for ACS in 16 hospitals across Malaysia. These patients were divided into two groups – elderly (≥ 65 years) and non-elderly (< 65 years). The clinical characteristics, treatment received (invasive or non-invasive) and outcomes (in-hospital and 30-day all-cause mortality) of the two groups were compared. The elderly patients were then grouped according to the type of treatment received, and the outcomes of the two subgroups were compared.
RESULTS
Elderly patients had a higher cardiovascular risk burden and a higher incidence of comorbidities. They were less likely to receive urgent revascularisation for acute ST-segment elevation myocardial infarction (elderly: 73.9% vs. non-elderly: 81.4%) and had longer door-to-needle time (elderly: 60 minutes vs. non-elderly: 50 minutes, p = 0.004). The rate of cardiac catheterisation was significantly lower in the elderly group across all ACS strata. Elderly patients had poorer outcomes than non-elderly patients, but those who received invasive treatment appeared to have better outcomes than those who received non-invasive treatment.
CONCLUSION
Elderly patients with ACS tend to be undertreated, both invasively and pharmacologically. Invasive treatment seems to yield better outcomes for this group of patients.
INTRODUCTION
According to the World Health Organization, ischaemic heart disease is the leading cause of death globally.(1) It is also a major cause of morbidity and mortality among the elderly.(2,3) With the increasing standard of general healthcare, the elderly population is expected to make up a large proportion of all acute coronary syndrome (ACS) patients in the future.
Age is an important determinant of outcome in ACS.(4,5) The elderly represents a subgroup of high-risk ACS patients due to their advanced age and the fact that they commonly have other comorbidities. Unfortunately, the elderly are also often sidelined and underrepresented in many clinical trials because of the aforementioned factors.(6) Due to the frailty and multiple comorbidities of elderly patients, physicians often face the dilemma of whether to perform aggressive invasive procedures on these patients. On the one hand, the use of aggressive invasive procedures may result in more harm being inflicted, but on the other hand, the elderly may benefit the most from aggressive treatment.
There is a paucity of data on elderly patients with ACS in Malaysia, where the rate of invasive coronary intervention is often limited by insufficient funding. Therefore, the present study aimed to examine the treatment attitude and clinical outcome of elderly patients with ACS by analysing data from the Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry.
METHODS
Anonymised patient data was obtained from the NCVD-ACS registry. The NCVD was sponsored by the Ministry of Health, Malaysia, and co-sponsored by the National Heart Association of Malaysia (NHAM).(7) The data of patients who were diagnosed with ACS (i.e. unstable angina, ST segment elevation myocardial infarction [STEMI] and non-ST segment elevation myocardial infarction [NSTEMI]) in 16 participating hospitals across Malaysia was captured in the NCVD-ACS registry. Using a standardised case report form, data was collected from the time the patient with ACS was admitted to the hospital till discharge from hospital, between 29 December 2005 and 26 April 2010. A unique national identification number was assigned to each patient to avoid duplication. Follow-up was done 30 days after hospital discharge via phone call or when the patient came to the clinic for a review. The patients' baseline characteristics and clinical presentation, in-hospital treatment, procedural details and clinical outcome were recorded. Data was entered into the NCVD website after verification. The operation of the NCVD is supported by a comprehensive information and communications technology system to ensure functional efficacy and effectiveness.
The patients were categorised into two groups – elderly patients (aged ≥ 65 years) and non-elderly patients (aged < 65 years). The cutoff age of 65 years was chosen based on our local practice; for example, age ≥ 65 years is the widely accepted age criterion for admission into a geriatric unit. The patients' ethnicity was determined based on self-report and the ethnicity stated on their national identity cards. In this context, STEMI was defined as persistent ST segment elevation ≥ 1 mm in two contiguous electrocardiographic leads, or the presence of a new left bundle branch block in the setting of positive cardiac markers. NSTEMI was defined as the occurrence of acute myocardial infarction in the setting of positive cardiac markers, with or without accompanying electrocardiographic changes other than ST-segment elevation. Unstable angina was defined as symptoms that were judged to be consistent with acute cardiac ischaemia within 24 hours of hospital presentation with serial cardiac markers negative for myocardial infarction.
Continuous variables were presented as mean ± standard deviation and differences among the ethnic groups were analysed using analysis of variance if the data was normally distributed. If the data was skewed, continuous variables were presented as median (interquartile range) and differences among the ethnic groups were analysed using Kruskal-Wallis test. Categorical variables were presented as number (percentage) and differences were analysed using chi-square test. Risk ratios were obtained using a generalised linear model with a log link, binomial distribution and a robust variance estimator. The risk ratios represent the relative risk of mortality for elderly patients as compared to non-elderly patients. Variables that showed a statistically significant difference (i.e. had a two-sided p-value < 0.05) between elderly and non-elderly patients in the univariate analysis and had clinical importance were adjusted for in the final model. Multicollinearity was assessed using the variance inflation factor. Risk ratios were considered statistically significant if their respective 95% confidence intervals excluded the value of 1. All statistical analyses were performed using Stata statistical software version 12.1 (StataCorp LP, College Station, TX, USA).
RESULTS
A total of 13,545 patients were included in the analysis. Most of these patients were male (78.4%) and of Malay ethnicity (49.0%). Among the 13,545 patients, 4,440 (32.8%) were elderly patients and 9,105 (67.2%) were non-elderly patients. The baseline characteristics of the elderly and non-elderly patients were compared, and the results are presented in
Table I
Baseline characteristics on admission according to age group.
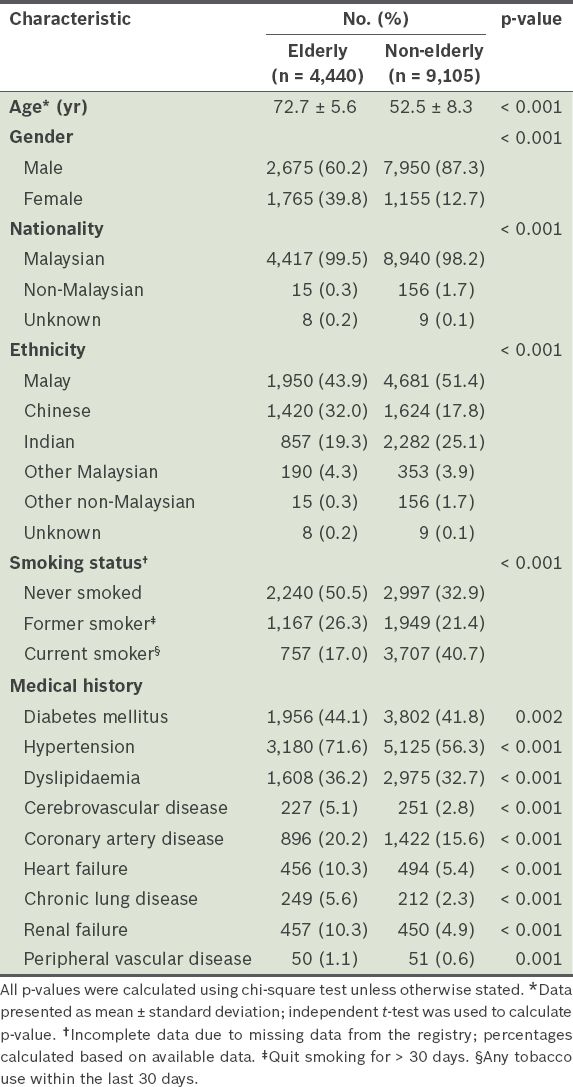
Elderly patients had a higher burden of cardiovascular risk factors. Compared to non-elderly patients, more elderly patients had a history of diabetes mellitus (41.8% vs. 44.1%), hypertension (56.3% vs. 71.6%) and dyslipidaemia (32.7% vs. 36.2%). Elderly patients also had a higher rate of comorbidities, as listed in
Table II
Acute coronary syndrome (ACS) diagnosis, presentation and acute treatment according to age group.
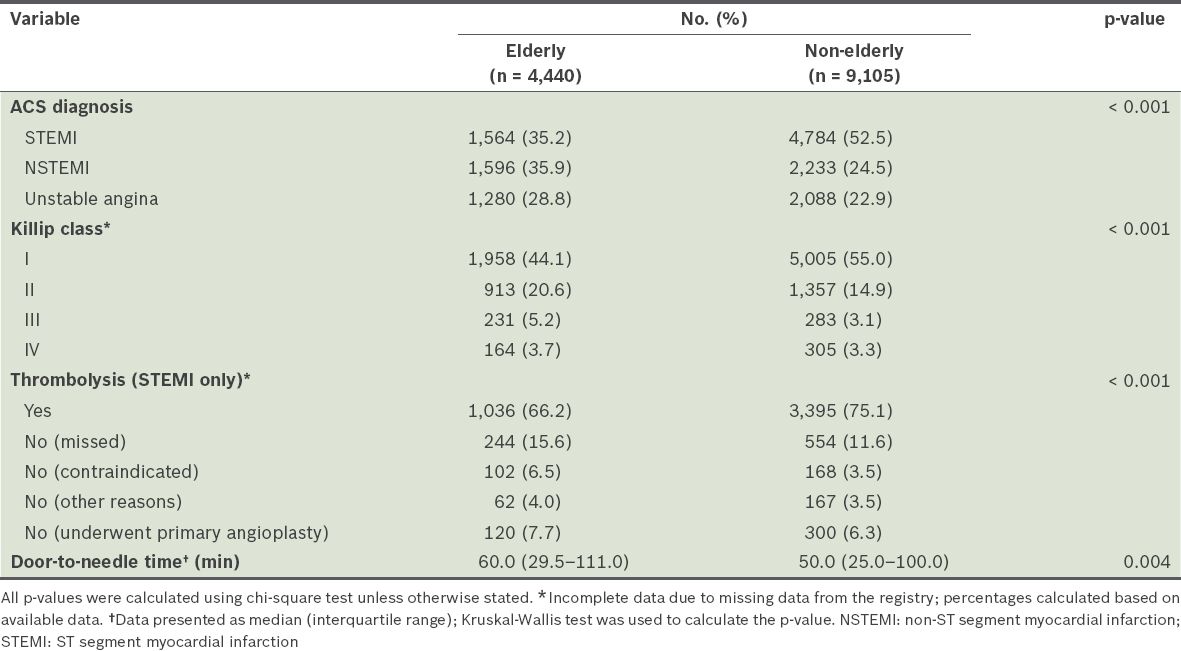
Table III
Treatment administered according to age group.
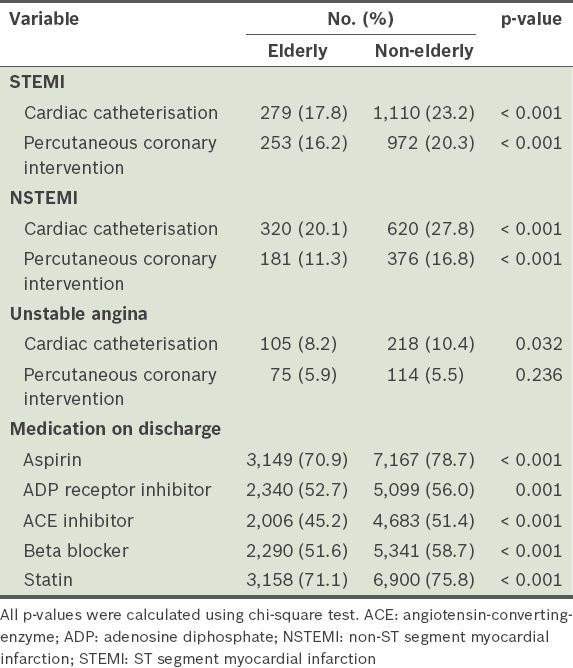
Comparison of in-hospital ACS management of elderly and non-elderly patients showed that elderly patients were given less aggressive treatment (both invasive and non-invasive therapy). In terms of invasive cardiac catheterisation, elderly patients clearly had a lower rate of cardiac catheterisation and PCI across all ACS strata. The rate of use of pharmacological therapy, in terms of all the essential drug groups, was also lower among elderly patients.
Table IV
Clinical outcome of patients according to age group.
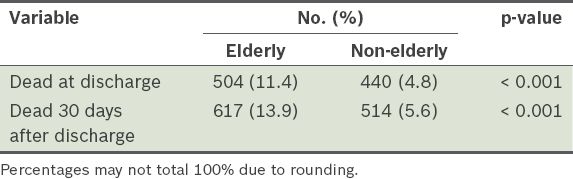
Table V
Adjusted risk of mortality at discharge (in-hospital) according to type of acute coronary syndrome.
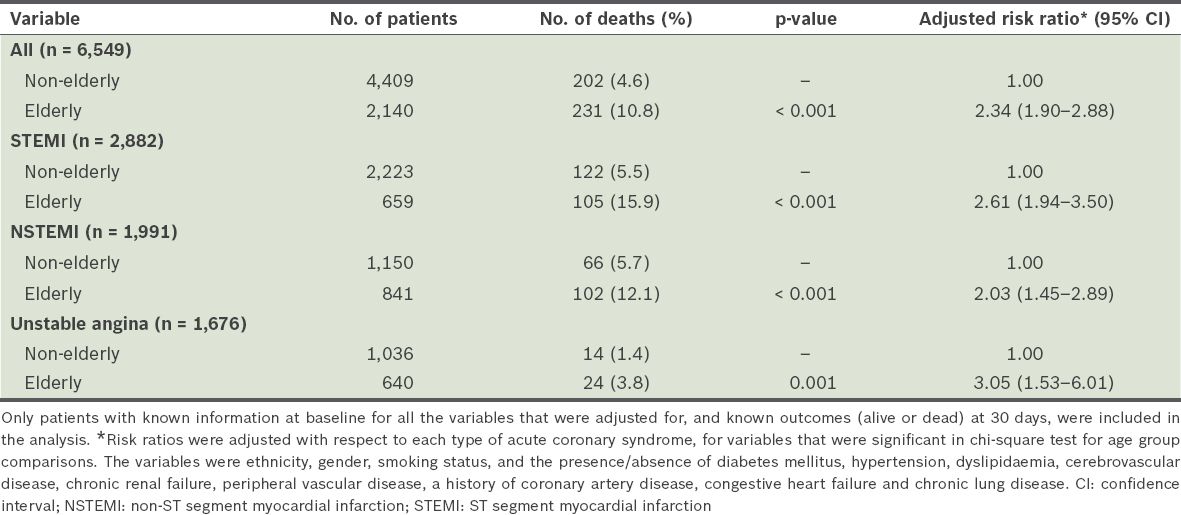
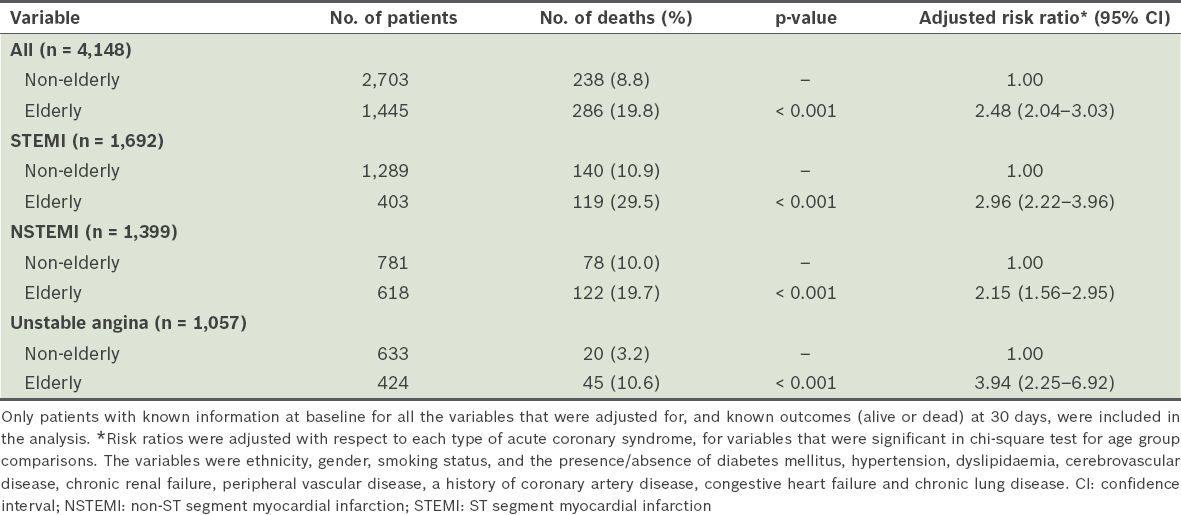
Table VI
Adjusted risk of mortality at 30 days after discharge according to type of acute coronary syndrome.
Tables
Table VII
Adjusted risk of mortality of elderly patients at discharge according to treatment invasiveness.
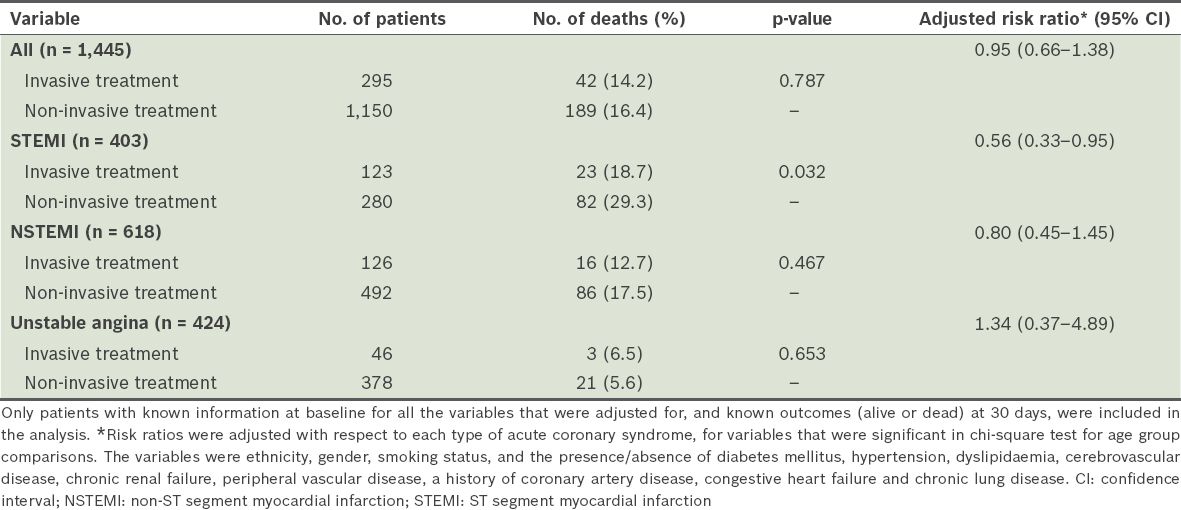
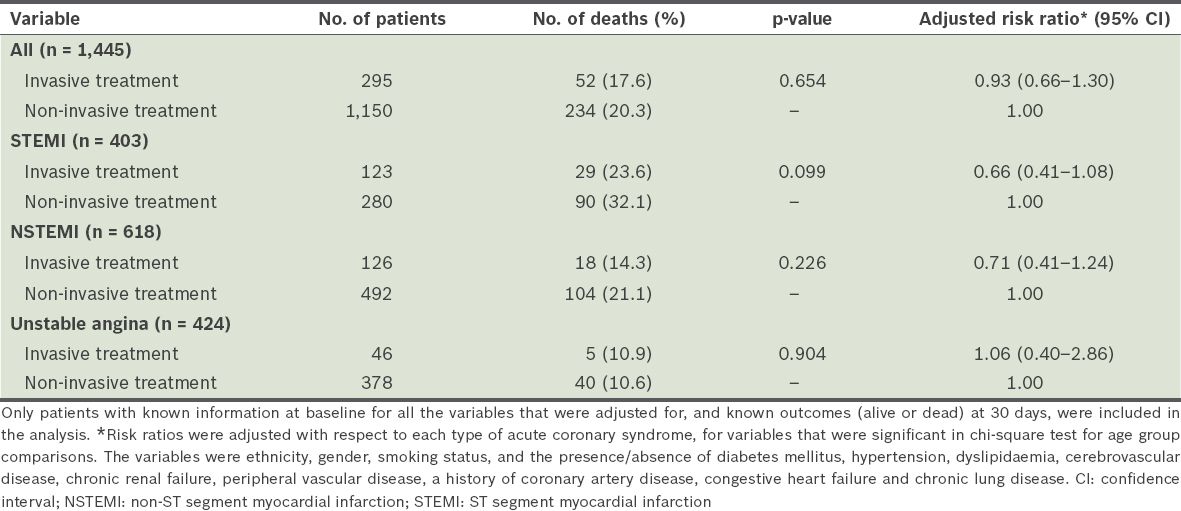
Table VIII
Adjusted risk of mortality of elderly patients at 30 days after discharge according to treatment invasiveness.
DISCUSSION
The Malaysian population comprises mainly Malays (50.4%), followed by Chinese (24.6%) and Indians (7.1%).(8) Malaysians have a high cardiovascular risk burden; according to the 2006 National Health and Morbidity Survey,(9) the prevalence of diabetes mellitus, smoking and hypertension among the Malaysian adult population was 11.6%, 46.5% and 42.6%, respectively. The elderly population in Malaysia is expected to continue growing to make up 9.8% of the total population by 2020.(10)
In the present study, elderly patients (i.e. aged ≥ 65 years) with ACS represent a group of patients who have a high burden of cardiovascular risk factors. Along with age as an independent predictor of cardiovascular mortality in ACS, these patients would be classified as "high-risk". Demographically, we found that there were significantly more individuals of female gender and Chinese ethnicity among the elderly patients than among the non-elderly patients. This finding is consistent with previous reports from the Southeast Asian region, which linked discrepancies in the age of onset for coronary artery disease with differences in ethnicity.(11-13)
In most of our institutions, pharmacological treatment for patients with ACS is still relevant, especially in the acute treatment of STEMI (e.g. intravenous thrombolysis). In most hospitals across Malaysia, intravenous thrombolysis remains the first-line treatment for acute STEMI (instead of primary PCI). This is due to limited funding and facilities for invasive treatment on a nationwide scale. However, PCI is still carried out in selected patients at the discretion of the cardiologist. We observed a discrepancy in the management of ACS between elderly and non-elderly patients. This discrepancy, although more marked in the rate of invasive procedures carried out, was also seen in the administration of pharmacological treatment. The percentage of elderly patients with STEMI who received reperfusion therapy (either intravenous thrombolysis or primary PCI) was lower than that of non-elderly patients (73.9% vs. 81.4%). Elderly patients also had a significantly longer door-to-needle time.
Age-related inequalities in ACS care are observed, even in the Western world where funding is less of an issue.(14,15) This is partly due to the delay in establishing a diagnosis among elderly patients due to their higher rate of atypical presentations. That is, ACS in elderly patients may go unrecognised at the initial point of consultation.(16) This discrepancy in care may be further compounded by the generally conservative attitude of physicians, especially toward invasive procedures, when treating elderly patients.(17) Studies have shown that orders for initial electrocardiography for elderly patients are often delayed and non-diagnostic in nature.(2,18) Other factors may also result in delays in treatment; for example, physicians may not understand the condition and incapacity of some elderly patients to make their own decisions. Elderly patients are often described as "double jeopardy" because not only are they likely to have longer door-to-balloon time, they are also less likely to be receptive toward receiving reperfusion and other evidence-based therapies.(19)
PCI is an established treatment for ACS; it helps to improve morbidity and mortality. Some earlier studies have shown that advanced age is associated with poorer short- and long-term outcomes in patients who have undergone PCI.(20-22) However, with advancements in PCI techniques, these outcomes may have changed. Newer data suggests that the outcome of PCI in elderly patients with acute myocardial infarction is comparable to that in younger patients.(23) In the present study, elderly patients had a higher burden of cardiovascular risk factors and comorbidities as compared to non-elderly patients. Also, we observed that, compared to non-elderly patients, elderly patients received significantly fewer aggressive treatments (both invasive and non-invasive) and had poorer outcomes at discharge and 30 days after discharge. The adjusted odds ratios of mortality for elderly patients and non-elderly patients are 2.34 (at discharge) and 2.48 (at 30 days after discharge), respectively. Elderly patients who were treated with invasive revascularisation by coronary angioplasty or coronary artery bypass grafting showed better outcomes than elderly patients who received non-invasive treatment. This suggests that age and comorbidities may not be a limiting factor in improving outcome by invasive cardiac revascularisation. Even if the outcome of elderly patients after PCI or coronary artery bypass grafting is not as good as that of non-elderly patients, there were still some mortality benefits to be gained from invasive treatment for elderly patients.
The present study illustrates the current treatment attitude toward the elderly and how elderly patients fare against younger patients. The results suggest that elderly patients likely are undertreated and receive suboptimal ACS management, especially in terms of invasive procedures that could be beneficial to them. Despite the higher rate of mortality seen among the elderly, they may still gain improvement in outcome if physicians adhere to ACS guideline-based therapy. Our results also support the recommendations of the American College of Cardiology/American Heart Association guidelines, which state that elderly patients should be evaluated using a similar standard as that used for younger patients for PCI candidacy, in deference to the patient's and his/her family's wishes.(24) Furthermore, our results are also consistent with the findings of previous studies on invasive coronary intervention among the elderly; multiple studies have shown that in the setting of STEMI, primary PCI would benefit patients from all age groups, including the elderly.(25-28) Similar results were seen for elderly patients with NSTEMI; those who were treated with early PCI revascularisation had better outcomes than those who were managed conservatively (i.e. non-invasive treatment).(2,4,29)
As the outcome of patients with ACS in our clinical setting is still far from satisfactory, efforts are currently being undertaken at a national level to improve the quality of care of patients. The Malaysian government has started increasing public awareness of the early symptoms of ACS, so as to shorten the symptom-to-door time, as well as expanding the number of cardiac catheterisation labs throughout the country in order to improve the rate of invasive revascularisation, especially in the setting of STEMI. We hope that more aggressive, evidence-based, pharmacological treatments will be administered to patients with ACS over the next few years, with resultant improvement in patient outcomes.
To conclude, although elderly patients with ACS are a subgroup of patients with high in-hospital and 30-day mortality risks, they tend to be undertreated (i.e. less invasive procedures and less aggressive pharmacological treatment). This may be due to the fact that elderly patients tend to be frail and have compounding comorbidities. However, the findings of the present study suggest that elderly patients treated with PCI have better outcomes than those who were treated with medical (non-invasive) therapy alone. Thus, there is evidence to suggest that PCI in the setting of ACS is still beneficial to elderly patients.
ACKNOWLEDGEMENTS
The authors would like to thank the physicians and nurses who participated in the Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome registry.


