CASE 1
CLINICAL PRESENTATION
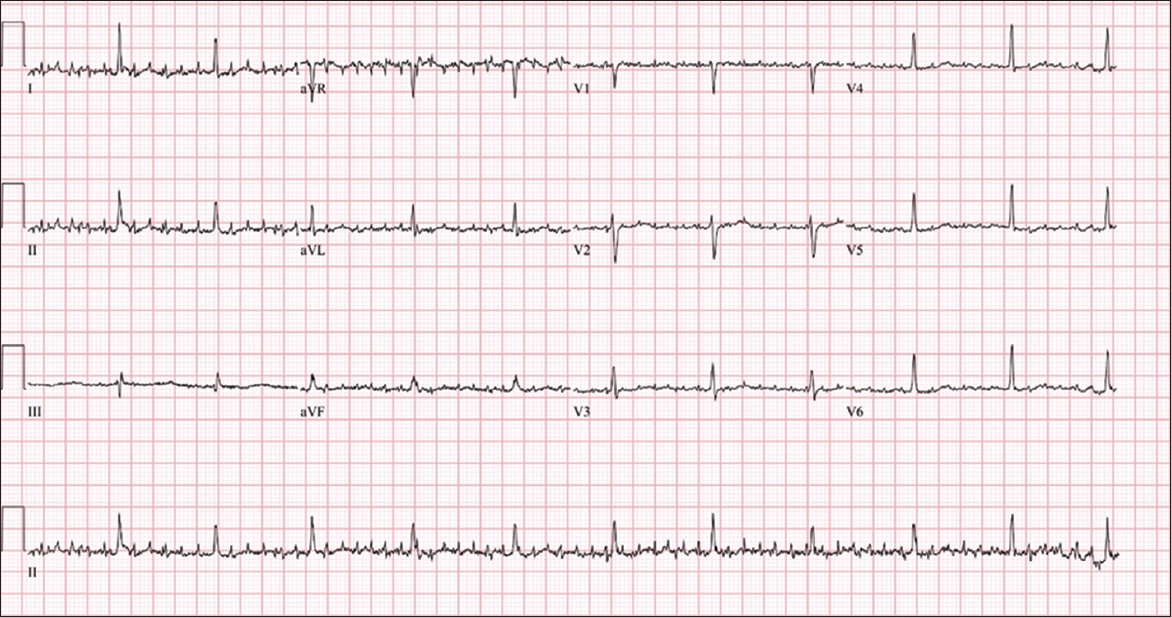
A 66-year-old woman with a past medical history of hypertension and left thalamic intracranial haemorrhage was reviewed in an outpatient clinic for persistent hypokalaemia with serum potassium levels of 2.8–2.9 mmol/L over a six-month period. Her family members reported that she was experiencing increasing lethargy. Physical examination showed a minimally communicative patient with the right arm contracted, increased tone and no right lower limb movement. An electrocardiogram (ECG) was obtained (
Fig. 1
Case 1: ECG of the patient on arrival.
ECG INTERPRETATION
The ECG in
CLINICAL COURSE
As the ECG revealed a diagnosis of atrial flutter (AFL), the patient was referred to the cardiology department. A repeat ECG after replacement of potassium demonstrated normal sinus rhythm with fewer movement artefacts.
CASE 2
CLINICAL PRESENTATION
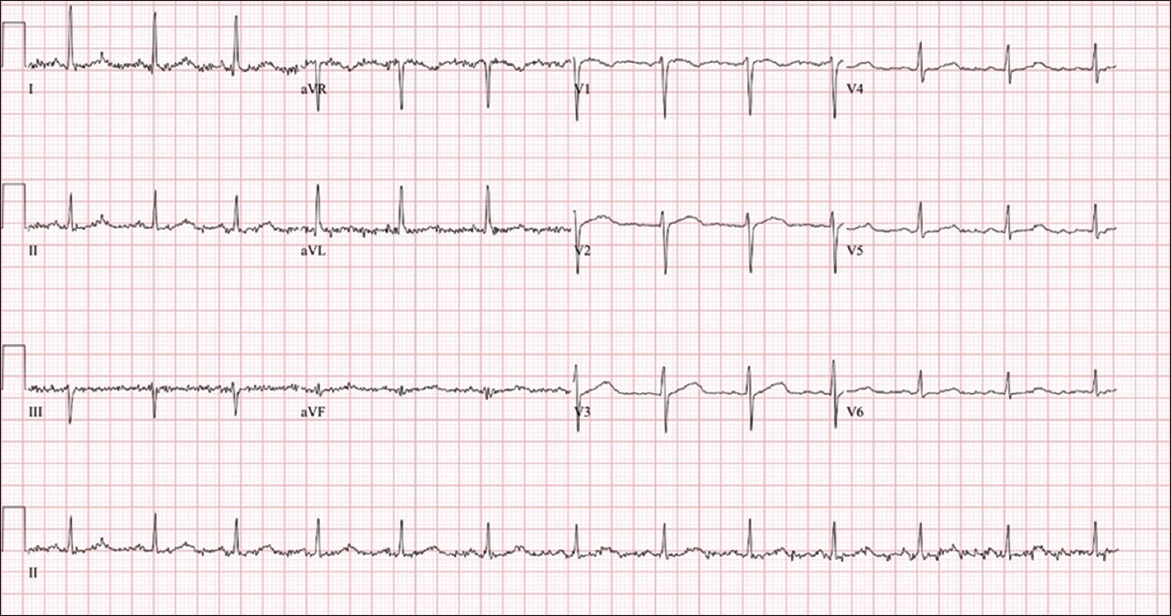
A 60-year-old Indian woman presented to the emergency department after a fall. She had a six-month history of right-sided resting hand tremors. Physical examination revealed right-sided coarse resting tremors with bradykinesia. An ECG (
Fig. 2
Case 2: ECG of the patient on arrival.
ECG INTERPRETATION
The ECG in
CLINICAL COURSE
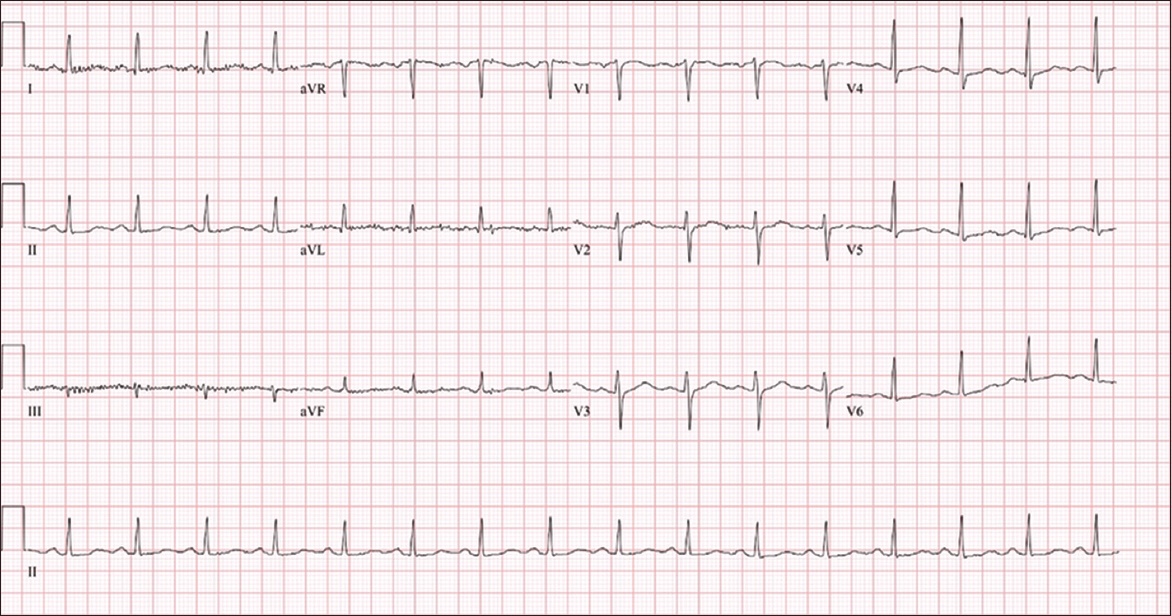
The patient was admitted to further evaluate the cause of her fall. An inpatient neurology review diagnosed Parkinsonism, and she was started on a dopamine agonist. Her tremor markedly improved upon initiation. A repeat ECG (
Fig. 3
Case 2: Repeat ECG shows resolution of artefacts.
DISCUSSION
Movement artefacts in movement disorders resulting in mimics of arrhythmia have been well described in Parkinson‘s disease (PD). A Parkinsonian tremor has a high probability of causing artefacts, and tremors with sufficient amplitude can lead to a misinterpretation of AFL, atrial fibrillation (AF) or even ventricular tachycardia (VT), as compared to those without.(1,2) The tremor in PD is 5–6 Hz, which translates to 300–360 cycles per minute, similar to the frequency at which a pseudoflutter can appear on an ECG. Hence, computer ECG interpretation may not be able to differentiate artefacts, with a tendency to misinterpret these artefacts as AFL.
Misinterpretation of artefactual ECGs as AF or AFL may lead to serious medical omissions and errors. Firstly, this may result in undertreatment of the precipitating neurological movement disorder or severe metabolic disturbance. Secondly, it can lead to unnecessary investigations such as echocardiography or overtreatment with anticoagulation for cardioembolic stroke prophylaxis.(3) For patients with suspected VT, this may include unnecessary intravenous infusions, cardioversions, electrophysiological studies and implantation of devices.(4) This highlights the importance of correct identification of a suspected arrhythmia.
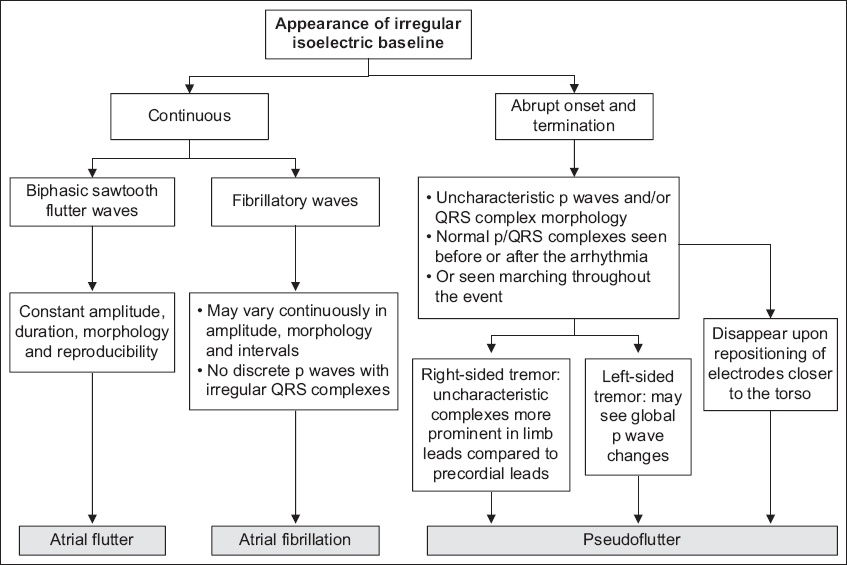
Various factors that can help to distinguish a pseudo-AFL from a true arrhythmia should be considered. Firstly, artefacts would be observed during periods of tremulousness (e.g. from shivering or seizure), with an abrupt onset during the tremor and termination when the tremor ceases.(4) Secondly, p waves may have uncharacteristic p wave and QRS complex morphologies with sharp contours. Normal complexes may also be seen before and after these periods of artefactual changes on ECG. Having a keen eye is useful in recognising these normal complexes that march in and out throughout the event. Thirdly, repositioning electrodes closer to the torso may help to minimise interference to the isoelectric baseline from limb movements. In a similar vein, we may notice that these artefactual changes are more prominent in limb leads than in precordial leads.(1) This can be appreciated in the ECGs of both Cases 1 and 2. However, one caveat is that in left-sided tremors, a prominent precordial flutter wave may be seen on the ECG, resulting in global p wave changes. It is suggested that this may be attributable to left limbs forming the negative composite pole of the precordial ECG waveform.(5) This serves as a reminder that ECGs should always be interpreted within the clinical context. The algorithm in
Fig. 4
Flowchart shows an algorithm to distinguish a pseudoflutter from true atrial fibrillation or atrial flutter.
Supplementary Material
SMJ-63-195.pdf


