Abstract
INTRODUCTION
The aim of this study was to determine the extent to which primary care doctors assessed patients newly diagnosed with hypertension for the risk factors of cardiovascular disease (CVD) during the patients’ first clinic visit for hypertension. The study also aimed to examine the trend of assessment for CVD risk factors over a 15-year period.
METHODS
This retrospective study was conducted between January and May 2012. Data was extracted from the paper-based medical records of patients with hypertension using a 1:4 systematic random sampling method. Data collected included CVD risk factors and a history of target organ damage (TOD), which were identified during the patient’s first visit to the primary care doctor for hypertension, as well as the results of the physical examinations and investigations performed during the same visit.
RESULTS
A total of 1,060 medical records were reviewed. We found that assessment of CVD risk factors during the first clinic visit for hypertension was poor (5.4%–40.8%). Assessments for a history of TOD were found in only 5.8%–11.8% of the records, and documented physical examinations and investigations for the assessment of TOD and secondary hypertension ranged from 0.1%–63.3%. Over time, there was a decreasing trend in the percentage of documented physical examinations performed, but an increasing trend in the percentage of investigations ordered.
CONCLUSION
There was poor assessment of the patients’ CVD risk factors, secondary causes of hypertension and TOD at their first clinic visit for hypertension. The trends observed in the assessment suggest an over-reliance on investigations over clinical examinations.
INTRODUCTION
Hypertension is a major public health concern. According to the World Health Organization, hypertension accounts for 4.5% of the global disease burden.(1) It has been predicted that by 2025, there will be a 60% increase in the number of hypertensive adult patients globally (from 972 million in 2000 to 1.56 billion).(2) Worldwide, the prevalence of hypertension varies from 5.2% to 70.7%.(3) In Malaysia, it is estimated that 43% of adults over the age of 30 have hypertension.(4)
Hypertension is associated with an increased risk of cardiovascular, cerebrovascular and renal diseases. This in turn leads to increased healthcare costs, which imposes substantial demands on national budgets. Many international and local clinical practice guidelines (CPGs) for hypertension have been published to help improve the quality of care for patients with hypertension and minimise healthcare burdens.(5-8) The Malaysian CPG for hypertension, first published in 1998, was revised in 2002 and 2008.(5-7) Most guidelines emphasise the importance of a thorough assessment for cardiovascular disease (CVD) risk factors, target organ damage (TOD) and secondary causes of hypertension when patients first present with hypertension.(5-7,9) Despite these efforts, one study has shown that up to 53% of patients with hypertension did not receive adequate CVD risk assessment.(10)
CVD risk factors, apart from hypertension, include advanced age (male ≥ 45 years, female ≥ 55 years), male gender, current cigarette smoking, a family history of myocardial infarction or sudden death (before the age of 55 years in a male parent or male first degree relative, and before 65 years in a female parent or female first degree relative), dyslipidaemia and diabetes mellitus.(11,12) Modifiable CVD risk factors should be actively managed in patients with hypertension to reduce their global cardiovascular risk.
Although hypertension is a very common condition in the primary care setting, little is known about the initial evaluation of hypertension performed in this setting. Therefore, the present study aimed to determine the extent to which primary care doctors assessed CVD risk factors in patients newly diagnosed with hypertension during their first clinic visit. The study also aimed to examine the trend of assessment for CVD risk factors over a 15-year period, from 1998 to 2012. This time period was chosen to coincide with the publication of the first edition of the Malaysian CPG for hypertension in 1998 and the second edition in 2002, and covers the four years after the publication of the third edition in 2008, so that we could examine if there was any correlation between our data and changes in the criteria of the Malaysian CPG for hypertension.
METHODS
This study was conducted at the University of Malaya Primary Care Clinic, an academic primary care practice in Malaysia. About 400–600 patients are seen daily at this clinic by a pool of 25–30 doctors, comprising family medicine trainees and trained family physicians. About a quarter of the patients had hypertension.
Our study was part of a larger study assessing adherence to CPGs for hypertension. Baseline data from the larger study was used in the present study. The medical records of all patients with hypertension who attended the clinic within a five-month period, between January and May 2012, were reviewed. Patients who were aged above 18 years and had been followed up at the clinic for hypertension for at least one year were included in the study. The paper-based records of these patients were then selected using a 1:4 systematic random sampling method. The records were reviewed and data on the patients’ first visit for hypertension was extracted. For the purpose of this study, a patient was taken to have hypertension if he had a diagnosis of hypertension in his medical records and/or was on antihypertensive medication.
An electronic, self-designed data collection form was used to record the patients’ sociodemographic characteristics and clinical data (e.g. CVD risk factors, TOD, secondary causes and investigation results) during their first clinic visit. If the presence or absence of a condition was documented in the medical records, it was noted as a ‘yes’ or ‘no’, respectively. If the condition was not mentioned in the records, it was noted as ‘not done’, even though the patient may have been evaluated for the condition with no documentation of the results.
Data collected included documentation of previous myocardial infarction, ischaemic heart disease, left ventricular hypertrophy, heart failure, stroke/transient ischaemic attack, peripheral vascular disease, renal impairment, diabetes mellitus, dyslipidaemia, smoking status, and family history of early cardiovascular death, ischaemic heart disease, hypertension, diabetes mellitus, renal impairment, stroke and dyslipidaemia. We also collected data from the patients’ physical examinations. This included information such as weight, height, peripheral pulses, carotid bruit, and the results of cardiovascular, respiratory, abdominal, and neurological and fundus examinations. The results of examinations for signs of endocrine disorders, such as Cushing syndrome, thyroid disorders and acromegaly, were also collected. In terms of investigations performed, results of the renal profile, uric acid, lipid profile, full blood count, fasting blood glucose, electrocardiography, chest radiograph, urine and microalbuminuria assessments were collected. Data collection was done by two trained research assistants.
Data analysis was performed using PASW Statistics version 18.0 (SPSS Inc, Chicago, IL, USA). Accuracy of the data was ensured via double data entry and a random audit of data by the researchers. Demographic data and rates of all the assessments at the first clinic visit were summarised using descriptive frequencies. Pearson’s chi-square test was used to examine the associations between categorical variables. In order to subanalyse patients with different CVD risks according to their gender and age (as recommended by the guidelines), the patients were categorised into: (a) a younger group, which included males aged < 45 years and females aged < 55 years (i.e. low risk); and (b) an older group, which included males aged ≥ 45 years and females aged ≥ 55 years (i.e. high risk).(11,12) Documentation of assessments performed for CVD risk factors (i.e. physical examinations and investigations) were also analysed over a time period that corresponded to the publication of the Malaysian CPGs for hypertension.(5-7) The documents were divided into three groups according to the dates of the patients’ first clinic visit for hypertension: Group 1 (February 1998–January 2002), Group 2 (February 2002–January 2008) and Group 3 (February 2008–May 2012). Frequencies of CVD risk factors were used to compare between the groups.
Ethics approval was obtained from the University of Malaya Medical Ethics Committee (Reference: 890.14). Data collected was anonymised to ensure patient confidentiality.
RESULTS
About 4,000 patients with hypertension attended the clinic during the study period and we reviewed the medical records of 1,060 patients. The mean age of the patients was 62.6 ± 10.5 years and the mean duration of hypertension was 8.5 ± 6.4 years. Only 5.5% of the patients were aged < 40 years at the time of their first visit to the clinic for hypertension. More than half of the patients were female (59.7%). The ethnic distribution was 48.0% Chinese, 30.5% Malay, 20.6% Indian and 0.9% other ethnicities.
Table I
Rates of documentation of history of cardiovascular disease (CVD) risk factors and target organ damage.
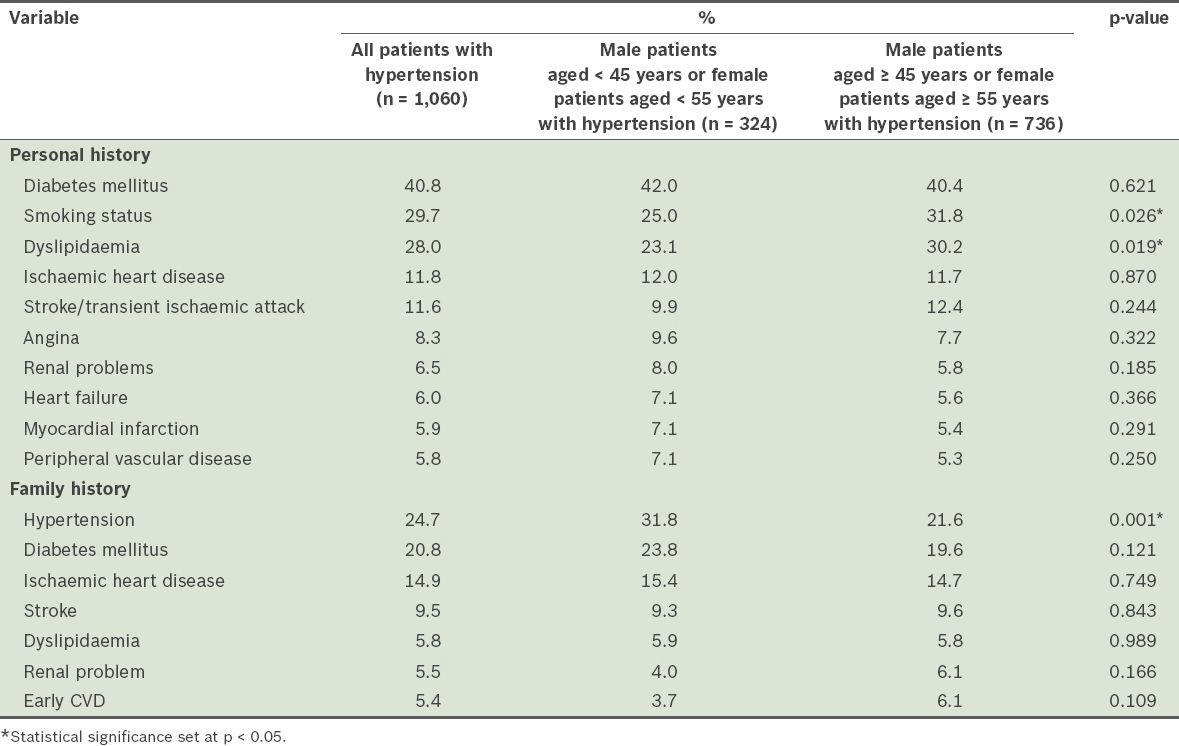
Table II
Rates of documentation of physical examinations and investigations.
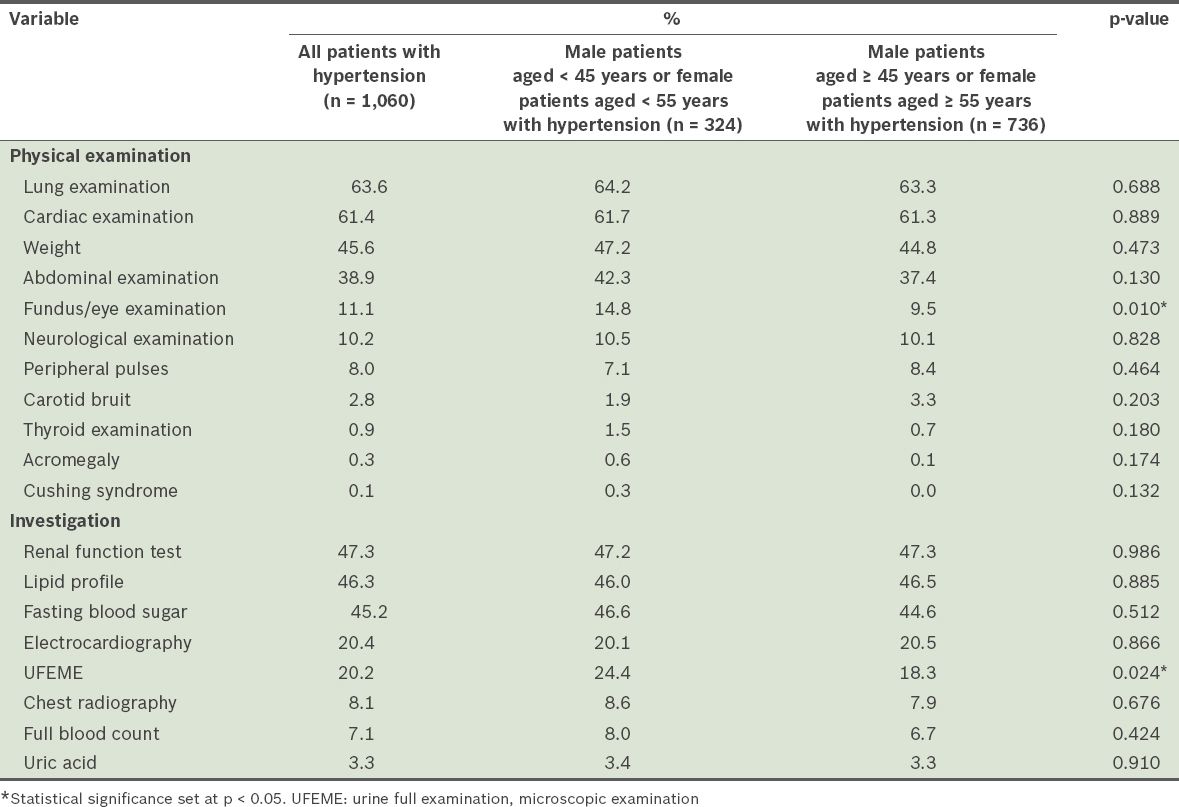
When the records of the older patients (i.e. male patients aged ≥ 45 years or female patients aged ≥ 55 years) were compared with those of the younger patients (male patients aged < 45 years or female patients aged < 55 years), Pearson’s chi-square test showed that the rates of assessment for a family history of hypertension, fundus examination and urinalysis were significantly higher among the younger patients. Older patients had significantly higher rates of assessment for smoking and dyslipidaemia as compared to the younger patients.
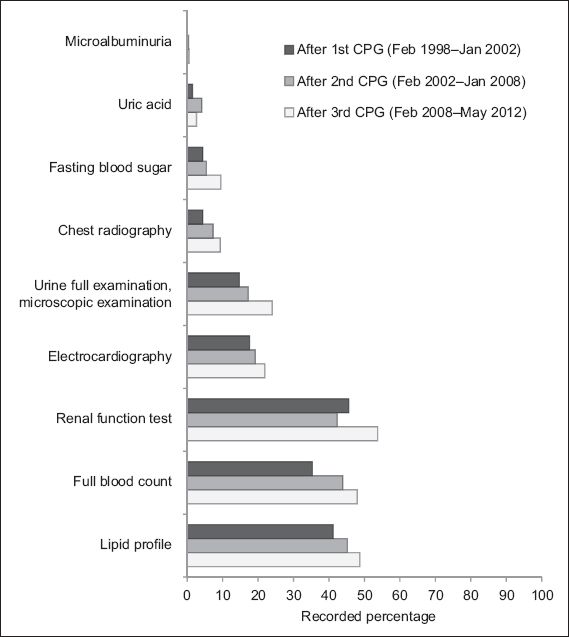
Figs.
Fig. 1
Bar graph shows the trend in the assessment of cardiovascular disease risk factors via physical examinations from 1998–2012, with the data categorised into time periods according to the publication/revision of the Malaysian clinical practice guidelines (CPGs) for hypertension.
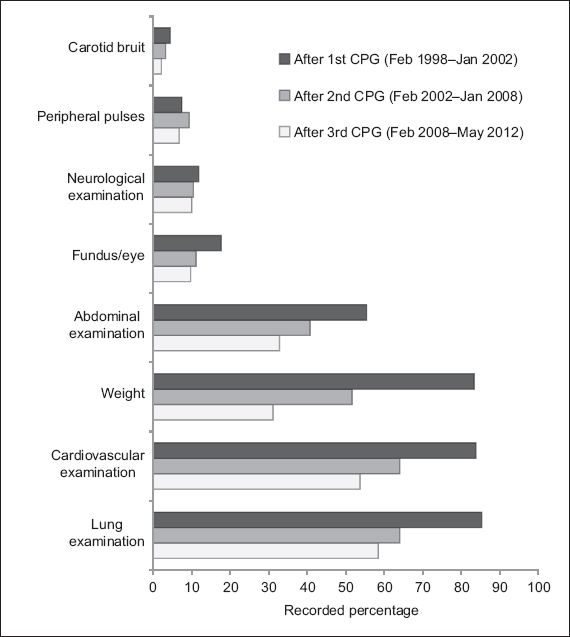
Fig. 2
Bar graph shows the trend in the assessment of cardiovascular disease risk factors via investigations from 1998–2012, with the data categorised into time periods according to the publication/revision of the Malaysian clinical practice guidelines (CPGs) for hypertension.
DISCUSSION
The results of the present study showed that there was poor assessment of patients’ CVD risk factors, secondary causes of hypertension and TOD during their first clinic visit for hypertension. This is similar to the findings of a study conducted in the United Kingdom(13) that suggested the presence of a gap in the clinical care for hypertension; in particular, missed opportunities to detect and prevent CVD and TOD. This gap could have a negative impact on the morbidity and mortality of such patients. Risk stratification for CVD is one of the most important components in the evaluation of patients with hypertension, as it helps to prevent future complications and determine the aggressiveness of the treatment required.(7,8)
The patient load in primary care is often heavy, resulting in short consultation times. In the present study’s setting, the patient load was worsened by the lack of an appointment system (i.e. patients were allowed to make unscheduled visits). It was also possible that the doctors assessed the patients without documenting the clinical data in their medical records. Adoption of an electronic health records system could be used as a means to improve documentation under such circumstances.(14) However, even in one study that used an electronic database, lipid investigations were only documented in a third of the patients.(15) Other studies have advocated the use of incentive systems, albeit with modest improvements in the quality of care.(16) There are other strategies to facilitate the adoption of CPGs, such as practice facilitation, interactive education and reminder systems.(17-21) Further research needs to be conducted to determine which strategy would be most effective in improving the process of care for hypertensive patients in the primary care setting.
Interestingly, in the present study, a greater proportion of the younger patients (i.e. males aged < 45 years and females aged < 55 years) had documented assessments of a family history of hypertension, fundus examination and urinalysis compared to the older patients (i.e. males aged ≥ 45 years or females aged ≥ 55 years). It is possible that the doctors were stratifying the possibility of secondary causes of hypertension (e.g. renal disease) and associating the patient’s family history of hypertension with essential hypertension in the younger patients. Up to 15% of all hypertension cases could be due to secondary causes.(22,23) Although the rate of secondary hypertension in younger patients is not known, it is still important to look for these secondary causes as they are potentially curable.
We found a decreasing trend in the percentage of documented physical examinations conducted and an increasing trend in the percentage of documented investigations conducted for the evaluation of hypertension during a patient’s first clinic visit. This suggests a decline in the use of clinical skills and an increased use of investigations in the assessment of CVD risk factors and TOD. In clinical practice, most diagnoses are attained through clinical assessment.(24,25) Only 4.8%–7.5% of diagnoses are attained through further laboratory testing.(24,26) Clinical skills, which include history-taking and physical examination, were once the primary means by which diagnosis and clinical monitoring were done. However, the findings of the present study indicate that these clinicians placed little importance on physical examinations and relied more on investigations for their assessment, as was observed elsewhere.(27)
The present study was limited by its retrospective design. Some doctors might not have documented negative findings in their records, leading to an underestimated rate of assessment. In addition, since the study was carried out in a single centre, the findings may not be representative of all medical facilities in Malaysia. Nevertheless, as the sample used was large and selected using systematic random sampling, our findings offer insights into the process of care of hypertensive patients in a primary care setting.
In the present study, we captured the baseline practice of doctors in a real-life setting and examined the impact of Malaysian CPGs on clinical practice over a 15-year period without intervention. In conclusion, there was poor assessment of CVD risk factors, secondary causes and TOD during the patients’ first clinic visit for hypertension. This could result in missed opportunities for early intervention to prevent morbidity and mortality due to CVD. The trends in assessment suggest an over-reliance on investigations over physical examination. Further research is required to explore the reasons for the levels of poor assessment and the decreasing practice of clinical examinations in primary care. Our findings will be used to develop an intervention that includes improved clinical workflow, use of record templates and training of healthcare providers to improve practice.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the doctors and staff of the Primary Care Clinic, University of Malaya, Kuala Lumpur, Malaysia. This study was funded by the Institute of Research Management & Monitoring University Malaya Research Grant RG335/11HTM.


