Abstract
A 59-year-old woman who had previously undergone an anatomic left total shoulder arthroplasty presented with increasing left shoulder pain and significant reduction in motion of the left shoulder joint. No evidence of prosthetic loosening or periprosthetic fracture was detected on the radiographs or fluoroscopic arthrogram images. Dual-energy computed tomography (DECT) images revealed evidence of loosening of the glenoid component and secondary rotator cuff failure. This case illustrates how a combination of detailed clinical history, careful physical examination and DECT arthrogram evaluation may be used to identify complications of an anatomic total shoulder arthroplasty.
CASE PRESENTATION
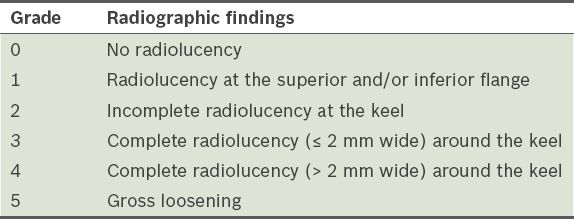
A 59-year-old woman presented with left shoulder pain and stiffness of 12 months’ duration. She had previously undergone an anatomic left total shoulder arthroplasty four years ago for avascular necrosis of the humeral head with advanced secondary glenohumeral osteoarthritis. The patient had actively participated in a postoperative rehabilitation programme, with good pain relief and restoration of function of the left shoulder. However, over a period of 12 months prior to the current clinical presentation, the patient began to experience increasing left shoulder pain and stiffness, which limited her activities of daily living. A physical examination revealed significant reduction in motion of the left shoulder, which included limitation of active forward flexion of about 40°. There was also difficulty in initiating shoulder abduction. Radiographic (
Fig. 1
Anteroposterior (a) radiograph and (b) fluoroscopic arthrogram image of the left shoulder. (c) Coronal and (d) sagittal monoenergetic 80 keV dual-energy computed tomography images of the left shoulder acquired immediately after the left shoulder arthrogram.
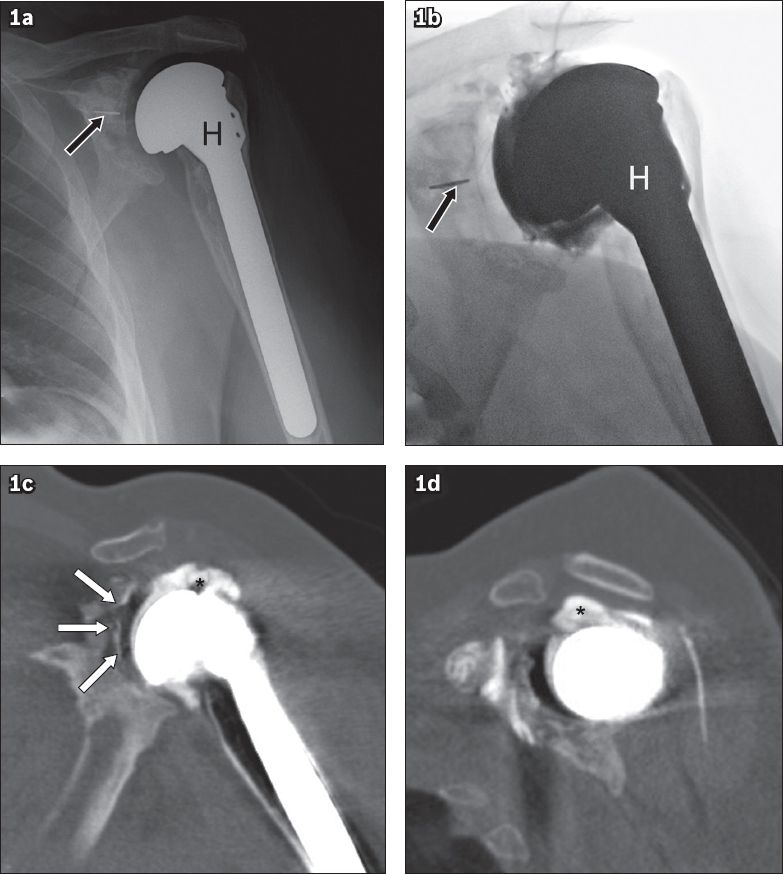
IMAGE INTERPRETATION
Anteroposterior radiography (
DIAGNOSIS
Total shoulder arthroplasty glenoid component loosening with secondary rotator cuff failure.
CLINICAL COURSE
In view of the left shoulder DECT arthrography findings of glenoid periprosthetic loosening and secondary rotator cuff failure, the patient was counselled on the need for further surgery. She declined surgery at that point in time, but was agreeable to undergo aspiration of the left shoulder joint, which excluded an underlying infection as a potential cause for the patient’s increasing shoulder pain. She has since been referred to a specialist pain management team for medical treatment of her left shoulder pain as a temporising measure.
DISCUSSION
Arthroses of the shoulder joint are common in ageing adults and can be debilitating due to the presence of significant pain and reduced range of motion of the shoulder joint, which results in an overall diminished quality of life.(1) Patients may be affected by primary osteoarthritis of the glenohumeral joint or have osteoarthritis secondary to preceding events such as trauma, avascular necrosis of the humeral head, inflammatory arthropathy, repetitive microtrauma in throwing athletes and joint instability. The exact incidence of glenohumeral osteoarthritis is not known, although Gartsman and Taverna found that approximately 13% of a total of 200 patients who underwent arthroscopy for full-thickness rotator cuff tears had coexisting chondral injuries.(2)
The majority of patients with glenohumeral osteoarthritis are treated with analgesics, which primarily consist of nonsteroidal anti-inflammatory drugs, with or without physical therapy. Intra-articular injections of steroids or viscosupplements such as hyaluronic acid have been found to provide temporary relief.(3) Surgical treatment options for glenohumeral osteoarthritis include arthroscopic debridement for chondral injuries, microfracture and osteochondral grafts, capsular release, and shoulder arthroplasty. Subacromial decompression may be indicated in a subset of patients with mild to moderate arthroses and concomitant impingement symptoms.(3)
Anatomic total shoulder arthroplasty, reverse shoulder arthroplasty, hemiarthroplasty and humeral head resurfacing are becoming increasingly more common in current orthopaedic reconstructive surgery practice. Approximately 27,000 total shoulder arthroplasties and 20,000 hemiarthroplasties were performed in the United States in the year 2008 alone.(4) Osteoarthritis was the primary indication in 77% of total shoulder arthroplasty cases and 43% of hemiarthroplasty cases. Proximal humeral fractures were the second most common indication for a hemiarthroplasty (33%).
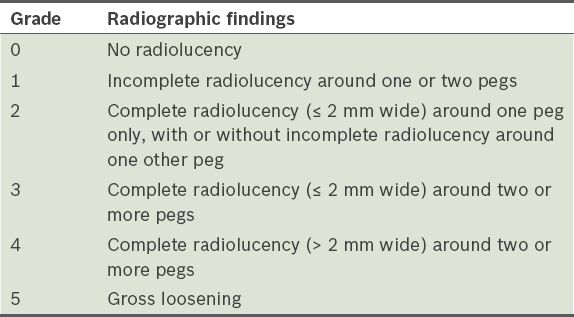
Our case involved an anatomic total shoulder arthroplasty, which is most commonly performed for degenerative osteoarthritis in patients older than 60 years, and required an intact rotator cuff. The humeral component is a minimally constrained anatomic implant consisting of a hemispherical metal articular surface and a cemented or press-fit stem. This articulates with a radiolucent polyethylene glenoid component. The central peg of the glenoid component contains a radio-opaque marker.(5) Pegged glenoid components (
Fig. 2
Illustrations show the (a) pegged and (b) keeled glenoid components used in shoulder arthroplasty (reproduced with permission from Lazarus et al(10)).
The most commonly encountered complication of anatomic total shoulder arthroplasty is loosening of the glenoid component, which occurs in up to 39% of patients following arthroplasty.(7) Preliminary imaging evaluation of the painful shoulder following an arthroplasty is typically performed using plain radiographs, where glenoid component loosening manifests as glenoid component migration, tilt or periprosthetic radiolucency measuring more than 1.5 mm in thickness.(7,8) The grading of periprosthetic radiolucency for keeled glenoid components was first described by Franklin et al (
Fig. 3
A 79-year-old man with prior anatomic total shoulder arthroplasty. Left shoulder radiograph shows periprosthetic lucency (arrows) related to the humeral component, which is in keeping with loosening.
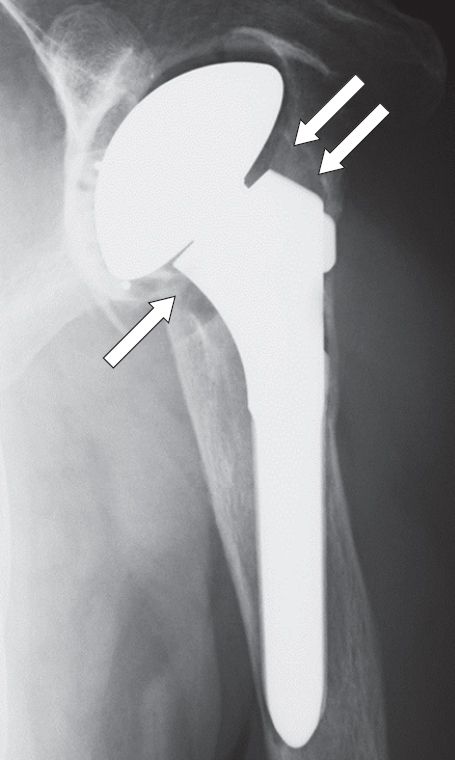
Fig. 4
An 81-year-old man with acute chronic left shoulder pain following arthroplasty. Lateral radiograph of the proximal left humerus shows periprosthetic lucency (black arrows), which is in keeping with loosening of the humeral component, and a cortical break close to the distal tip of the stem (white arrow), which is compatible with a periprosthetic fracture.

Fig. 5
A 53-year-old man with previous arthroplasty who presented with acute left shoulder pain and restricted range of motion following a fall. Axial left shoulder radiograph shows loss of congruency between the articular surfaces of the glenoid (G) and humeral (H) components secondary to acute posterior dislocation.
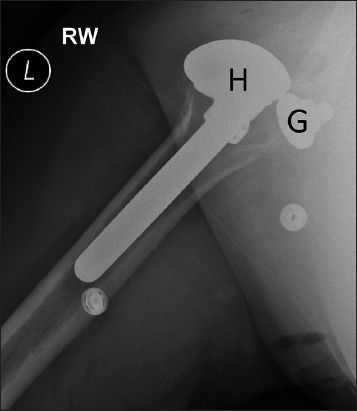
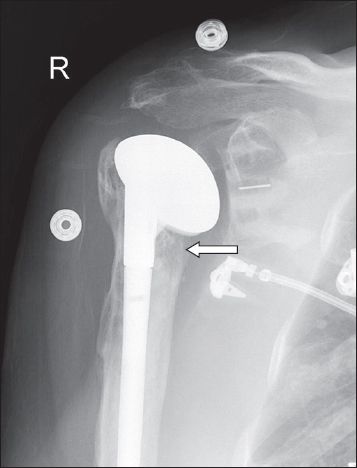
Fig. 6
A 79-year-old woman with increasing shoulder pain following shoulder arthroplasty. Anteroposterior radiograph shows increased lucency and early erosion inferior to the prosthetic humeral head (arrow). US-guided aspiration of the shoulder joint was performed and cultures of the aspirated joint fluid were positive for infection.
Implant loosening may also be evaluated using CT, although image degradation caused by significant metal artefacts may prevent reliable analysis of implant fixation.(12,13) New CT protocols and image reconstruction techniques have been developed in an attempt to reduce these artefacts,(14,15) although further studies are required to evaluate the true efficacy of these techniques in the context of shoulder arthroplasty. Insinuation of intra-articular contrast medium into the bone-cement or implant-cement interface is also diagnostic of loosening of the glenoid component. While Mallo et al concluded from their study of 14 patients that CT arthrography (CTA) had a high positive predictive value of 87.5% in the diagnosis of glenoid component loosening, they also urged caution in predicting component stability based solely on a negative CTA study, particularly in view of the low negative predictive value of 50%.(16)
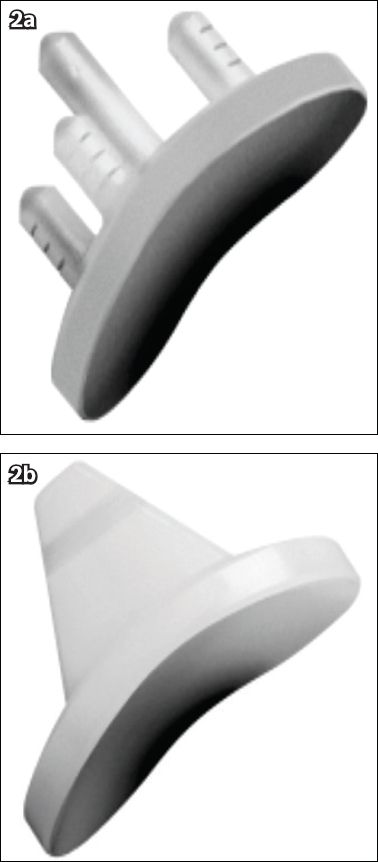
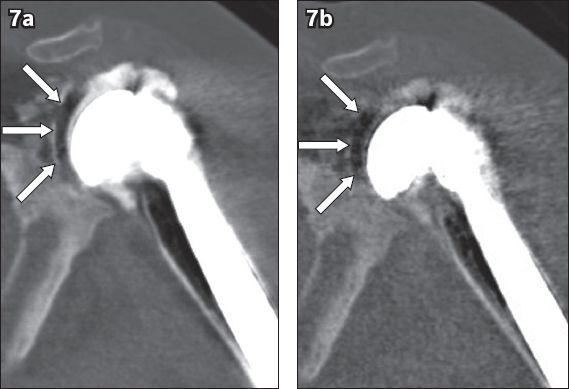
Utilisation of the monoenergetic spectrum of DECT to minimise beam hardening artefacts associated with implanted metal orthopaedic devices is an important application in musculoskeletal imaging.(17) The image quality and diagnostic value of DECT imaging of orthopaedic hardware were found to be significantly improved, with minimal artefacts, at a high-energy monoenergetic 130 keV setting.(18,19) This was seen in our case, where monoenergetic 130 keV images were superior to average weighted 120 keV images in minimising beam hardening artefacts (not shown). Of note, the monoenergetic 80 keV images better demonstrated contrast insinuation into the implant-cement interface (which confirmed the presence of glenoid component loosening) compared to the monoenergetic 130 keV images (
Fig. 7
Coronal monoenergetic (a) 80 keV and (b) 130 keV DECT images of the left shoulder. The sliver of contrast insinuating into the implant-cement interface of the glenoid component (arrows) is better demonstrated in the 80 keV than the 130 keV DECT image.
The integrity of the rotator cuff is typically evaluated using ultrasonography, which has been found to be a highly accurate imaging modality for evaluating the integrity of the rotator cuff following shoulder arthroplasty.(21,22) Prickett et al found that ultrasonography had a sensitivity of 91%, specificity of 86% and accuracy of 89% for identifying rotator cuff integrity postoperatively.(22) In our case, the DECT shoulder arthrogram was also useful in determining the presence of a full-thickness rotator cuff tendon tear (a known complication of anatomic total shoulder arthroplasty), in addition to the finding of glenoid component loosening. The finding of a full-thickness rotator cuff tendon tear is important, as it influences further surgical management of the patient; a reverse total shoulder arthroplasty was one of the options considered as a salvage procedure, rather than a simple revision of the loosened glenoid component, given the presence of secondary rotator cuff failure.(11) A reverse total shoulder arthroplasty differs from an anatomic total shoulder arthroplasty in that the humeral component consists of a proximal cup-shaped portion (with radiolucent polyethylene insert) and metal stem, while the ‘glenoid’ component consists of a hemispheric metal component (glenosphere) that attaches to a baseplate (metaglene), which is itself secured to the native glenoid using screws (
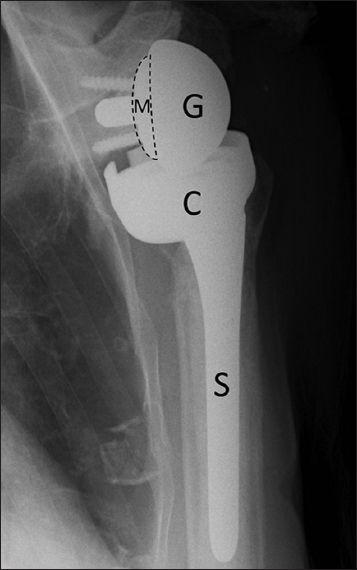
Fig. 8
Reverse total shoulder arthroplasty in a 76-year-old woman. Anteroposterior radiograph of the right shoulder shows the humeral component, which consists of a stem (S) and cup-shaped proximal portion (C). The glenosphere (G) is a hemispheric metal component that articulates with the humeral cup via a radiolucent polyethylene insert. The glenosphere is attached to a baseplate known as metaglene (area marked with broken lines; M), which is fixed on the native glenoid using screws.
In scenarios where plain radiography, ultrasonography or CT fail to identify the underlying cause of the patient’s symptoms, magnetic resonance (MR) imaging may be performed to further evaluate for potential pathology or address a specific clinical question.(23) Compared to plain radiography or CT, MR imaging is able to provide a superior assessment of the soft tissue structures surrounding the shoulder joint, which include the rotator cuff, deltoid muscle, neural structures, joint capsule and synovium.(23) Osteolysis, implant loosening and wear-induced synovitis may also now be evaluated using MR imaging due to advances in metal artefact suppression imaging techniques.(23)
Notwithstanding the availability of different imaging modalities that have been shown to be useful in the evaluation of a patient with symptoms following total shoulder arthroplasty, the case we have presented illustrates how a DECT arthrogram may be used to identify glenoid component loosening, the most commonly encountered postoperative complication, particularly when preliminary plain radiographic findings are not conclusive. Knowledge of the other potential complications of a total shoulder arthroplasty, as described in this article, will also greatly aid the managing clinician and reporting radiologist in the postoperative imaging evaluation of an anatomic total shoulder arthroplasty.
SMJ-57-177.pdf