Abstract
A 46-year-old Chinese woman with a history of cholecystectomy and appendicectomy presented to the emergency department with symptoms of intestinal obstruction. Physical examination revealed central abdominal tenderness but no clinical features of peritonism. Plain radiography of the abdomen revealed a grossly distended large bowel loop with the long axis extending from the right lower abdomen toward the epigastrium, and an intraluminal air-fluid level. These findings were suspicious for an acute caecal volvulus, which was confirmed on subsequent contrast-enhanced computed tomography (CT) of the abdomen and pelvis. CT demonstrated an abnormal positional relationship between the superior mesenteric vein and artery, indicative of an underlying intestinal malrotation. This case highlights the utility of preoperative imaging in establishing the diagnosis of an uncommon cause of bowel obstruction. It also shows the importance of recognising the characteristic imaging features early, so as to ensure appropriate and expedient management, thus reducing patient morbidity arising from complications.
CASE PRESENTATION
A 46-year-old Chinese woman presented to the emergency department with nausea and abdominal bloating, accompanied by vomiting that had increasingly worsened over the past four days. Apart from previous laparoscopic cholecystectomy and open appendicectomy, she had no other medical comorbidities. Physical examination revealed abdominal distension with central tenderness and active bowel sounds. There was no rebound tenderness or abdominal guarding. She was afebrile and her haemodynamic parameters were stable. Initial blood investigations revealed an elevated total white blood cell count of 15.9 (normal range [NR] 4.0–10.0) × 103/uL and a raised serum lactate level of 2.28 (NR 0.5–1.0) mmol/L. Arterial blood gas results were pH 7.45 (NR 7.35–7.45); partial pressure of carbon dioxide (pCO2) 28.6 (NR 35.0–45.0) mmHg; and standard bicarbonate 22.2 (NR 21.0–27.0) mmol/L, suggesting the presence of partially compensated primary respiratory alkalosis with no evidence of primary metabolic acidosis.
Plain radiography of the abdomen (
Fig. 1
(a) Supine (left) and erect (right) plain radiographs of the abdomen. Contrast-enhanced (b) coronal and (c) axial CT images of the abdomen and pelvis.
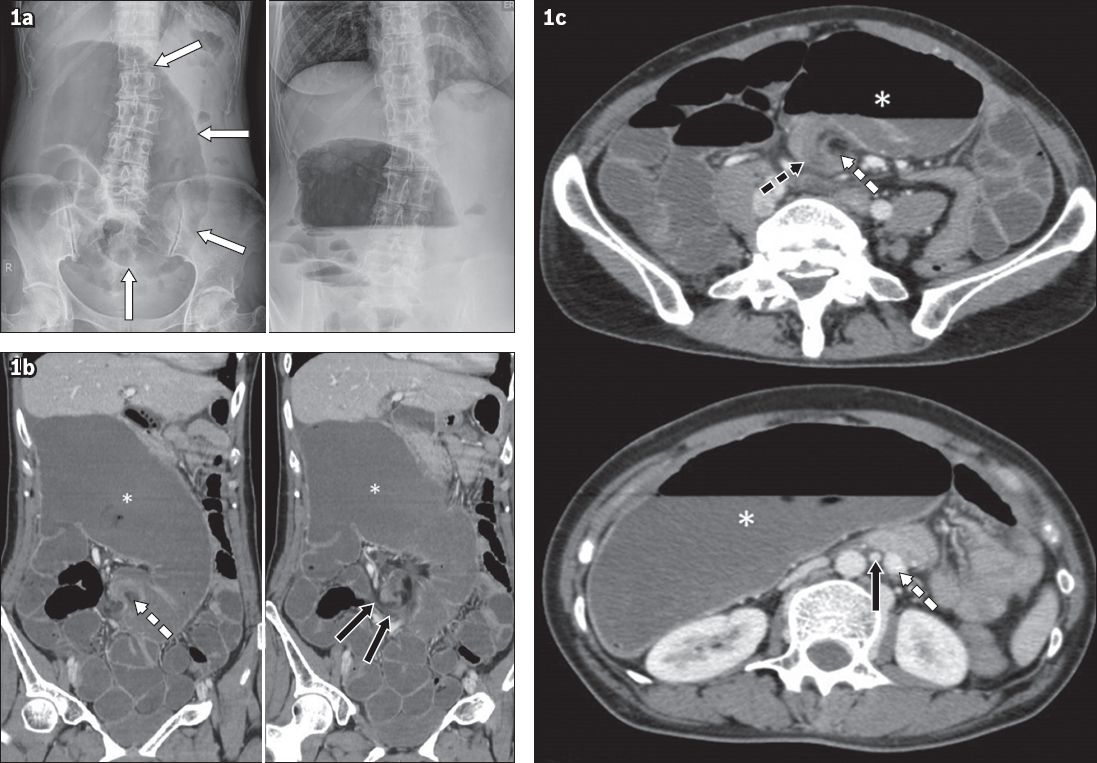
IMAGE INTERPRETATION
Plain radiographs (
DIAGNOSIS
Caecal volvulus with underlying intestinal malrotation.
CLINICAL COURSE
The patient was operated on emergently due to the risk of colonic perforation. The findings of caecal volvulus with serosal tears and punctate perforation of the ascending colon were confirmed intraoperatively (
Fig. 2
Intraoperative photograph of the grossly dilated caecum with evidence of a serosal tear (white arrow).

DISCUSSION
Caecal volvulus is an uncommon cause of bowel obstruction, with an estimated incidence of 2.8–7.1 per million people per year, accounting for 1%–1.5% of all adult intestinal obstructions and 25%–40% of all cases of colonic volvulus.(1) Although the aetiology of caecal volvulus is often thought to be complex and multifactorial, excessive caecal mobility is a commonly implicated factor.(2,3) This is thought to be due to incomplete intestinal rotation during embryonic development, resulting in inadequate or abnormal fixation of the right hemicolon.(4) Other contributory factors include prior abdominal surgery, late-term pregnancy, and high fibre intake or chronic constipation. These factors presumably cause increased caecal displacement or hyperperistalsis.(2,5)
Clinically, patients tend to present with recurrent intermittent abdominal pain or acute intestinal obstruction. Close to half of patients who present with acute obstruction due to caecal volvulus have a history of preceding recurrent intermittent abdominal pain that is localised to the right lower quadrant of the abdomen. They may develop high-pitched bowel sounds and focal tenderness during symptomatic episodes that resolve spontaneously. Clinically, acute intestinal obstruction due to caecal volvulus is often indistinguishable from other causes of acute bowel obstruction. Hence, imaging investigations are useful adjuncts in diagnosis.
Although CT is often the best imaging tool in the diagnosis of caecal volvulus,(5) plain radiography is usually the first-line imaging investigation used in the evaluation of central abdominal pain.(2) Therefore, it is important to recognise radiographic abnormalities that are identifiable in nearly all patients who present acutely with intestinal obstruction due to caecal volvulus. These include caecal dilatation (seen in 98%–100% of cases), a dominant intraluminal air-fluid level (72%–88%), dilatation of the small bowel (42%–55%) and a paucity of gas in the distal colon (82%).(1) Despite the high sensitivity of radiographic evaluation, it lacks the specificity conferred by CT imaging in the diagnosis of caecal volvulus, and patients are not uncommonly misdiagnosed as having small bowel obstruction.
The ‘CT coffee bean’, ‘bird beak’ and ‘whirl’ signs are three common CT findings that are associated with acute caecal volvulus. The ‘CT coffee bean’ sign generally refers to an axial view of a dilated caecum filled with air and fluid that may be visualised anywhere within the abdominal cavity. It should not be confused with the radiographic ‘coffee bean’ sign associated with sigmoid volvulus. The ‘bird beak’ sign refers to progressively tapering efferent and afferent bowel loops pointing to the site of torsion, which resemble bird beaks. The ‘whirl’ sign on a CT image describes a soft-tissue mass with internal architecture that contains swirling strands of soft tissue and fat attenuation. In the setting of acute caecal volvulus, the ‘whirl’ is composed of a spiralled loop of collapsed caecum with low-attenuating fatty mesentery and engorged mesenteric vessels.(6) A variant of caecal volvulus called the caecal bascule has also been described. This is a rare form of caecal obstruction caused by folding of the caecum anterior to the ascending colon, resulting in a ‘flap valve’ that occludes caecal emptying without true twisting; caecal bascule is responsible for 10% of all cases of caecal obstruction.(7,8) Patients with caecal bascule tend to have a better prognosis and lower incidence of vascular compromise of the bowel. An abnormal positional relationship between the superior mesenteric vein and artery, indicative of intestinal malrotation, is also identifiable on CT.(9) Contrary to normal anatomy, the vein is located to the left of the artery.
Treatment options for caecal volvulus include endoscopic reduction and surgery. Endoscopic reduction only has a success rate of approximately 30% and is generally considered ineffective.(10) The general consensus, therefore, is that surgical management of caecal volvulus is recommended, with the exact surgical approach depending on the intraoperative findings. Bowel resection is preferred when there is evidence of bowel gangrene or impending perforation, as seen in our patient. Non-resectional surgery, such as caecopexy or caecostomy, is generally less invasive and may be considered in the absence of bowel ischaemia. Residual hypermobility of the right hemicolon after caecal-sparing surgery has been implicated as a cause for the high recurrence rates of caecal volvulus, which were previously reported to be up to 40% for caecopexy and 33% for caecostomy tube placement.(1)
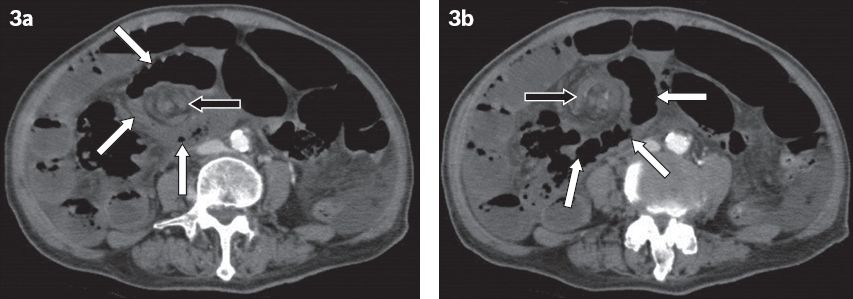
Intestinal malrotation is also a major predisposing factor for midgut volvulus. As compared to cases of caecal volvulus in which there is inadequate or abnormal fixation of the right hemicolon, midgut volvulus occurs when there is abnormal fixation of the small bowel mesentery, resulting in an abnormally short mesenteric root.(11) Plain radiography findings in cases of midgut volvulus are nonspecific and seldom helpful in establishing a definitive diagnosis. Fluoroscopic upper gastrointestinal and small bowel studies are useful in demonstrating the characteristic features of midgut volvulus, namely the abnormal position of the small bowel in the right side of the abdomen and that of the ligament of Treitz (indicative of malrotation), as well as the corkscrew-like appearance of the small bowel if midgut volvulus is present.(12) Knowledge of the CT findings of midgut volvulus is also important; the preoperative diagnosis is often made based on cross-sectional imaging, given that most patients present with nonspecific symptoms. Aside from the aforementioned abnormal positions of the small bowel and ligament of Treitz, other characteristic CT findings include swirling of the mesenteric root vessels at the site of the volvulus (
Fig. 3
Intestinal malrotation complicated by midgut volvulus and bowel ischaemia in a 46-year-old woman who presented with abdominal distension and vomiting of four days’ duration. (a & b) Contrast-enhanced axial CT images show swirling of the mesenteric root vessels (black arrows) and small bowel (white arrows) at the site of the volvulus. Note the non-enhancing mesenteric root vessels at the site of the volvulus, as well as diffuse non-enhancement of the small bowel loops, which is consistent with extensive bowel ischaemia.
In conclusion, it is imperative to recognise the imaging features of caecal volvulus early, so as to ensure appropriate and expedient management, and thus reduce patient morbidity from potential complications. CT is more specific when compared to radiography and has become the imaging modality of choice for establishing a preoperative diagnosis of caecal volvulus and distinguishing this condition from other causes of intestinal obstruction.
SMJ-57-602.pdf


