Abstract
INTRODUCTION
This study explored and compared the differences in attitudes toward end-of-life care among patients, relatives and healthcare professionals, including doctors and nurses.
METHODS
We performed a descriptive study on a cross-section of the population of a tertiary hospital in Singapore. Data was collected using a questionnaire survey involving 50 participants from each of the four groups of patients, relatives, doctors and nurses.
RESULTS
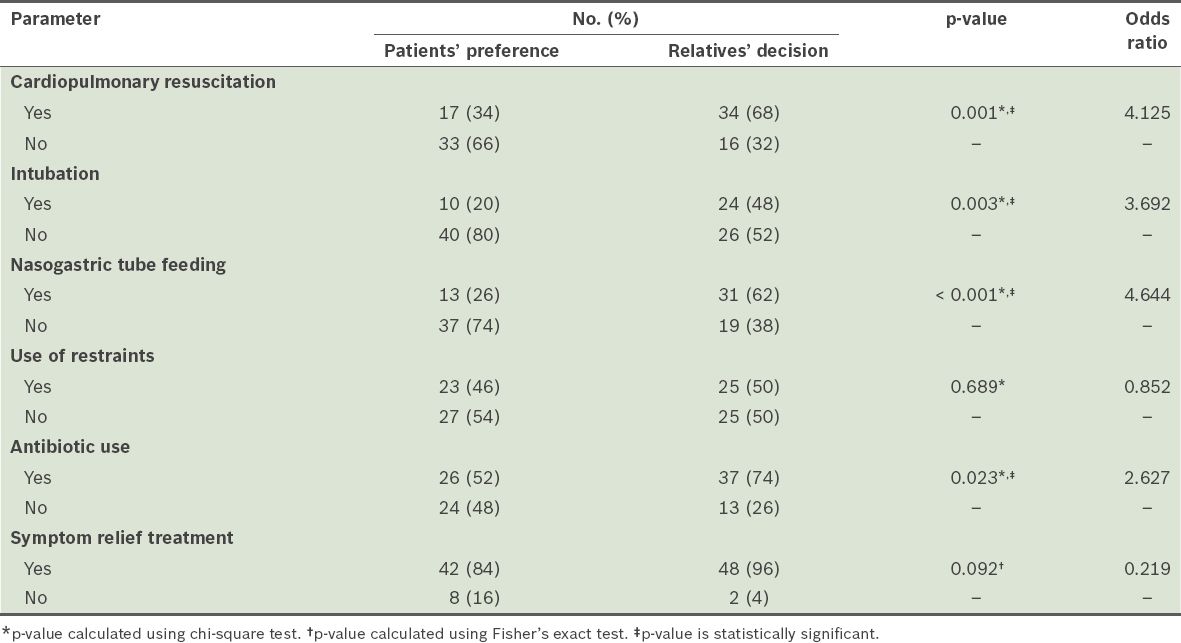
Family members were the most commonly nominated surrogate decision-makers by the patient group (76%) and the majority of the relative group (74%) felt comfortable deciding on end-of-life care for their loved ones. However, the patient and relative groups differed significantly in their preferences on end-of-life care options, including cardiopulmonary resuscitation (CPR) (p = 0.001), intubation (p = 0.003), nasogastric tube feeding (p < 0.001) and the use of antibiotics (p = 0.023). Doctors, nurses and relatives demonstrated differences in preference between end-of-life care for themselves and for their loved ones, especially with regard to the use of nasogastric tube feeding. There was also a difference between patients and doctors in their decisions on CPR (p < 0.001) and intubation (p = 0.008).
CONCLUSION
This study demonstrated the importance of early planning for end-of-life care. This must be initiated proactively by healthcare professionals to engage patients in a culturally sensitive manner to discuss their preferences, in order to facilitate open communication between the patient and family.
INTRODUCTION
Like all successful developed nations, within the next 20 years, a substantial proportion of Singapore’s population will consist of elderly residents. The Population Trends 2015(1) report has shown a consistent increase in the percentage of residents aged 65 years and above from 1970 to 2015, rising to an age dependency ratio of 16.2%. Singapore is a multicultural society that is predominantly made up of close-knit families with strong family ties, its members choosing to live close to one another. Next-of-kin often participate in decision-making in different aspects of medical care, with elderly members of the family unit relying on their children to make decisions for them. However, many Singaporeans have not talked about death and dying with their loved ones.(2) The reluctance to make end-of-life decisions for dependent elders stems from the pain of the imminent loss, guilt and/or helplessness associated with their decision.(3)
End-of-life care is a term used to describe support for people who are approaching death.(4) This concept and practice is relatively new, and represents a continuously evolving and improving branch of medical care that physicians in Singapore are trying to adopt.(5) Most are still unfamiliar with this concept, and uncomfortable with initiating discussion on and providing end-of-life care.(6) In contrast to life-sustaining technological progress in medicine, making decisions about end-of-life care for another human being places a heavy responsibility on the decision-maker. As a challenging aspect of the medical profession, it also strains hospital resources, and results in psychological and financial stress for patients and their families. Any decision between prolonging life at all costs and dignified end-of-life care will always be difficult for both physicians and the patients’ family members. Hence, education which addresses attitudes and cultural prejudices regarding end-of-life care is crucial for equipping physicians and enabling family members to understand and evaluate the pros and cons of their options in order to make the most appropriate decision.
To reduce the gap between their respective expectations, physicians need a better understanding of the cultural perceptions as well as personal preferences and attitudes of the relatives and next-of-kin, while the next-of-kin require an informed understanding of the financial, psychological and mental costs of prolonging life. The increased practical knowledge will better prepare relatives and next-of-kin to minimise emotional decisions, thus avoiding artificially prolonging life unnecessarily. To facilitate this process, our study aimed to explore and compare differences in the attitudes, preferences and decision-making surrounding end-of-life care among patients, relatives, doctors and nurses.
METHODS
This descriptive study examined a cross-section of a population in Changi General Hospital, a tertiary hospital in Singapore, from June 2012 to December 2012. The population was made up of elderly patients, relatives, nurses and doctors. Data was collected from four groups – patients, relatives, doctors and nurses – and a convenience sampling method was adopted, with 50 participants in each group. The patients and their relatives were all able to communicate coherently in English and/or Mandarin and were recruited from the geriatric outpatient clinic. The doctors and nurses were from the Geriatric Medicine and General Medicine departments. The principal researcher explained the study to the potential participants and was on-site to clarify any questions. Verbal consent was obtained and participants were assured of confidentiality.
The study was conducted using a survey questionnaire consisting of two parts. The first part contained demographic data with variables such as age, gender, race, religion and educational level. The second part comprised two scenarios that asked participants to imagine themselves or a loved one, respectively, becoming permanently uncommunicative and completely dependent in self-care. The questions explored preferences on end-of-life care, including the preferred place of death; the use of cardiopulmonary resuscitation, intubation, nasogastric tube feeding, use of restraints, antibiotics and symptomatic treatment; and decision-making on end-of-life care with regards to the preferred decision-maker and level of comfort in decision-making. The questionnaire aimed to answer four questions: (a) what was the preference of patients/relatives/doctors/nurses on end-of-life care for themselves?; (b) what were doctors’/nurses’/relatives’ attitudes to end-of-life care for their loved ones?; (c) what were the differences between their preferences/choices on end-of-life care made for themselves and their loved ones?; and (d) what was the difference between patients’ own preferences and their relatives’ preferences on their behalf?
Data was analysed using IBM SPSS Statistics version 19.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used to analyse and present the quantitative data, including demographic variables of the participants and their response to questionnaire items involving their attitude toward end-of-life care. Chi-square test and Fisher’s exact test were performed to compare differences in participants’ attitudes toward end-of-life care. A p-value < 0.05 indicated statistical significance for all the tests.
RESULTS
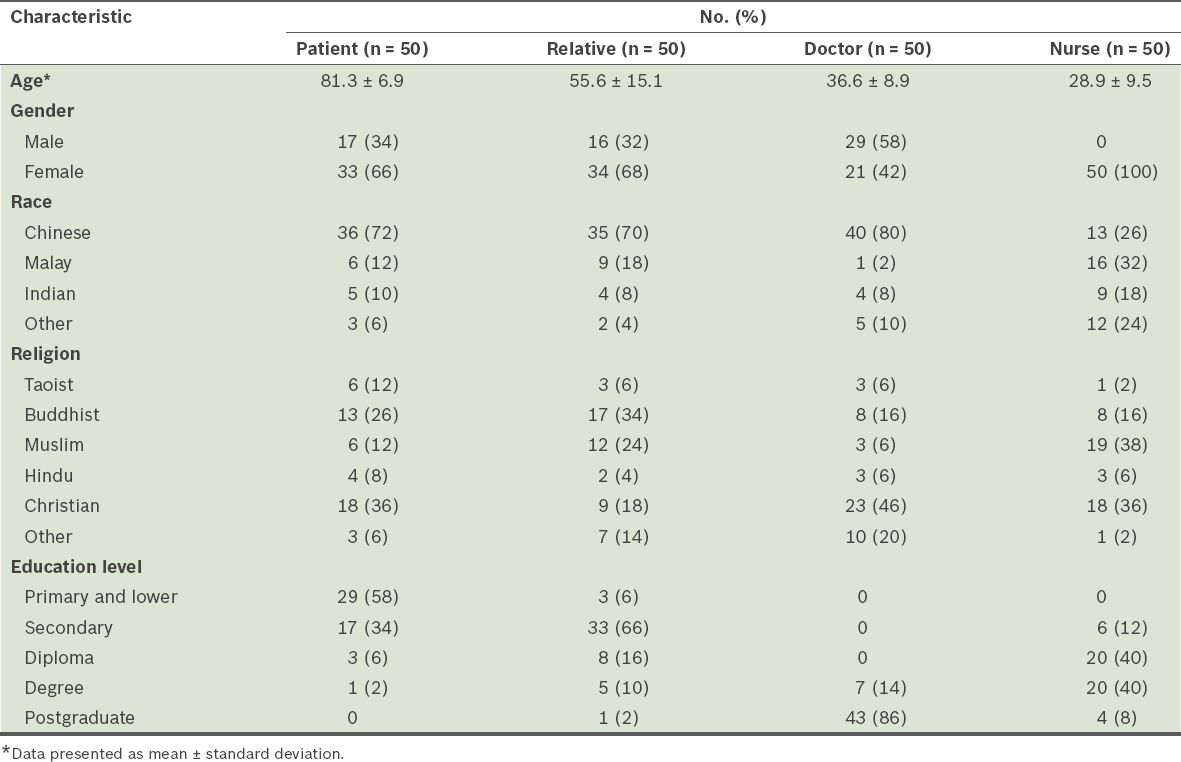
The mean age of the participants was 50.6 (range 19–94) years. The patients had the oldest mean age of 81.3 ± 6.9 years, while the nurses had the youngest mean age of 28.9 ± 9.5 years, compared to that of the relatives (55.6 ± 15.1 years) and doctors (36.6 ± 8.9 years). The ratio of male to female participants was about 1:2. The majority were Chinese (n = 124, 62%) and had attained secondary school-level education and higher (n = 168, 84%). Notably, most patients had only an educational level of primary school or lower (n = 29, 58%). The demographics of the study population are shown in
Table I
Demographic data of participants.
Of the 200 participants, 82% (n = 164) chose home as their preferred place at time of death (
Table II
Comparison of preference on end-of-life care by age group.
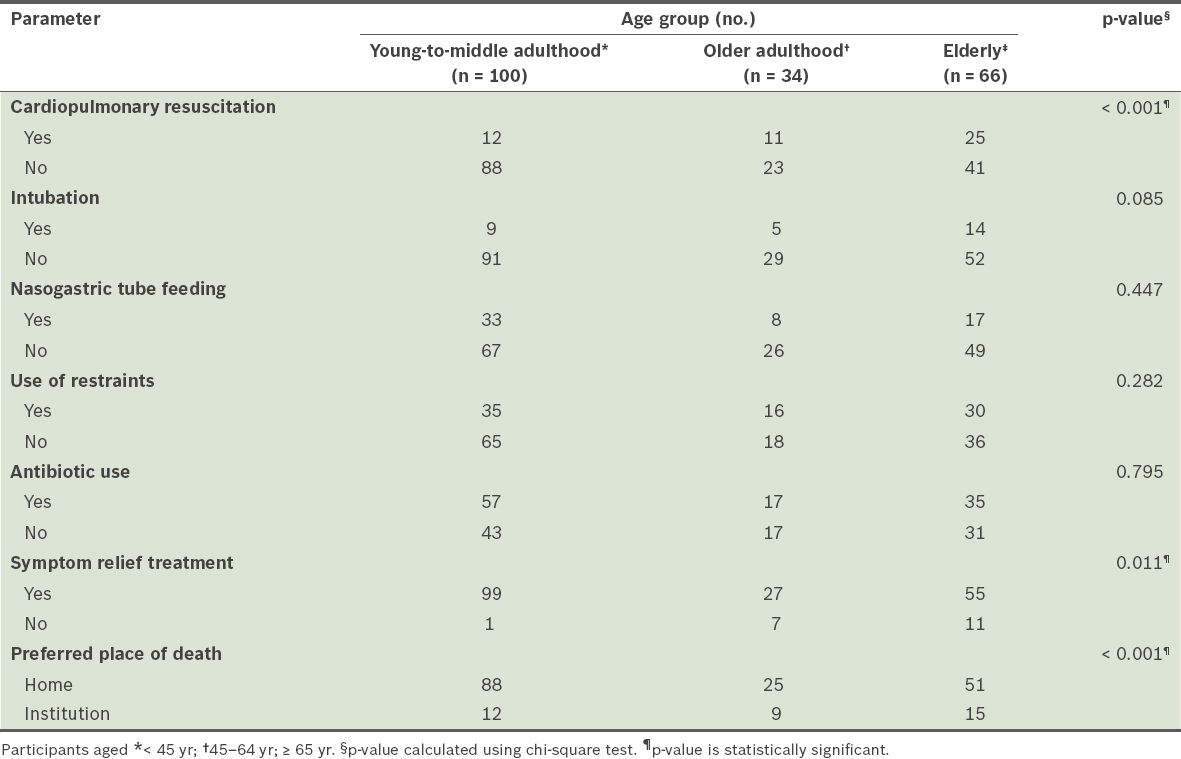
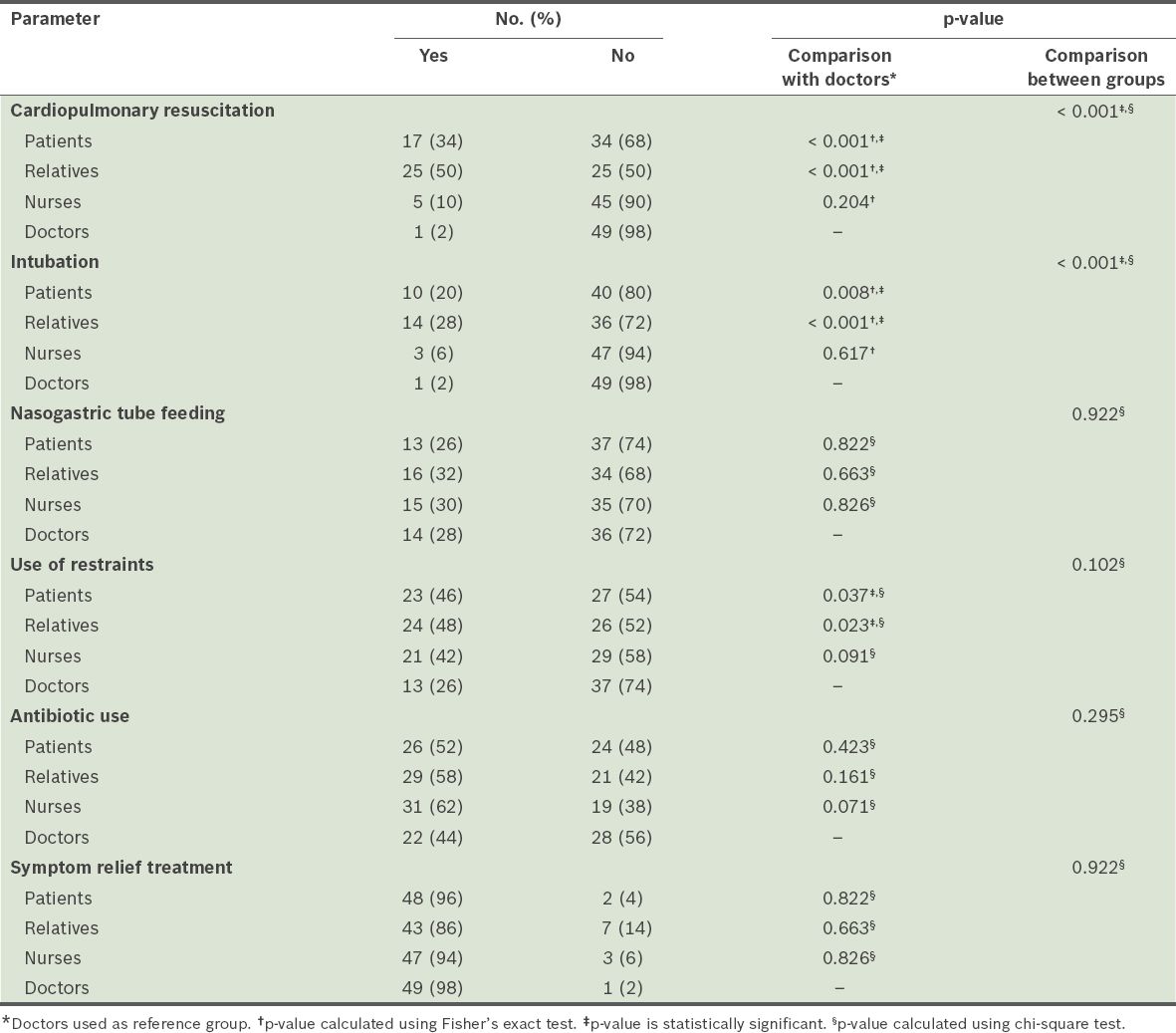
Table III
Comparison of patients, relatives, doctors and nurses’ attitudes toward end-of-life care for themselves (n = 200).
When participants’ attitudes toward end-of-life care were analysed by age group, without considering their roles, significant differences were observed in their responses toward CPR, symptom relief treatment and preferred place of death. The participants who were in young to middle adulthood (< 45 years) were less likely to prefer CPR (p < 0.001), but more likely to prefer symptom relief treatment (p = 0.011) and home as place of death (p < 0.001) than those in older adulthood (age 45–64 years) and the elderly (65 years of age or older) (
Most participants in the relative (n = 36, 72%), nurse (n = 44, 88%) and doctor (n = 43, 86%) groups also regarded home as the preferred place of death for their loved ones. The majority of relatives (n = 37, 74%) felt comfortable with being the surrogate decision-makers for their loved ones. However, relatives, nurses and doctors demonstrated a significant difference in their decision on the use of CPR (p < 0.001), intubation (p < 0.001) and antibiotics (p = 0.026) for their loved ones. More relatives (n = 34, 68%) preferred their loved ones to be given CPR than the doctors (n = 3, 6%) and nurses (n = 13, 26%). There were also more relatives (n = 24, 48%) who said they would opt for intubation on behalf of their loved ones compared to doctors (n = 5, 10%) and nurses (n = 9, 18%). Notably, those in the relative (p = 0.003), nurse (p = 0.041) and doctor (p = 0.039) groups were all more likely to opt for nasogastric tube feeding for their loved ones than for themselves. More relatives preferred their loved ones to undergo intubation (n = 24, 48%) than subject themselves (n = 14, 28%, p = 0.039) to that care option; similarly, nurses preferred antibiotic treatment for their loved ones (n = 42, 84%) more than for themselves (n = 31, 62%, p = 0.013).
A comparison of attitudes toward end-of-life care among the doctor, nurse and relative groups is shown in
Table IV
Comparison of doctors, nurses and relatives’ attitudes toward end-of-life care for their loved ones.
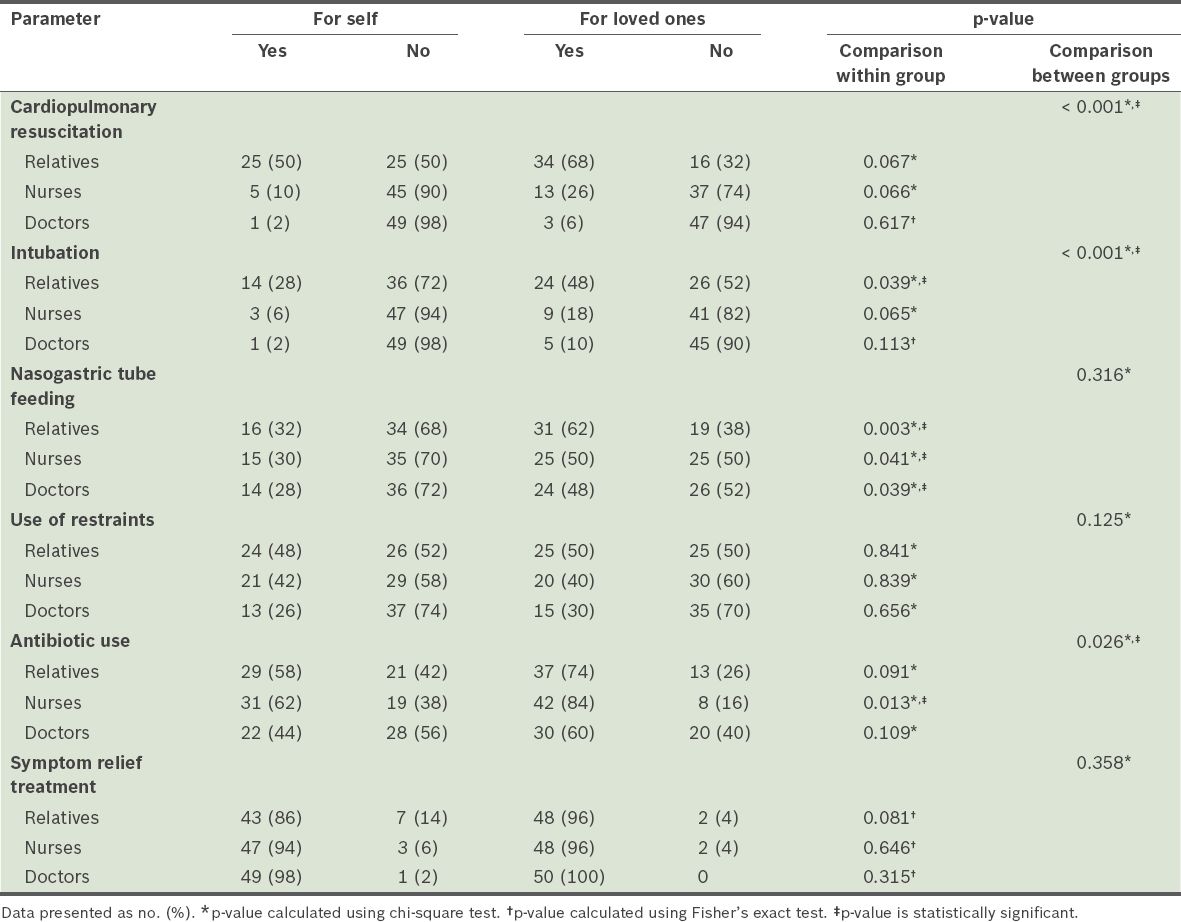
Table V
Comparison between patients’ own preference and relatives’ decision for their loved ones.
DISCUSSION
Ascertaining patients’ end-of-life wishes is a challenge for physicians in their daily practice due to the emotions of the patients and their families, possible complexity of the illness and advances in life-sustaining treatments. There is a fine balance between making medically and ethically fair decisions, and fulfilling the wishes and expectations of patients and relatives. The principle of autonomy that is well-accepted in developed Western countries might not be applicable to the local context. In Singapore’s population of mixed Asian ethnicities, collective decision-making by the family unit is a widely accepted cultural norm. Doctors often have to tread carefully between respecting the family’s preference for protective nondisclosure for the patient and their duty of care to the patient, which requires including the patient in decision-making and disclosing end-of-life care options to terminally ill patients.(7,8) Based on this study, most people would want the option to decide on their family member’s treatment instead of leaving the choice solely to the physician. In addition, they may also be concerned about the eventual medical costs of the treatments, but do not broach the subject for fear of being labelled as uncaring and money-minded.(9)
Not surprisingly, most patients, relatives, doctors and nurses choose the home as their preferred place of death. This finding shows that more community service providers should facilitate death at home to fulfil the desire of the dying person, and make available an additional hospital bed. However, more elderly participants indicated that their preferred place of death was an institution, including nursing homes, hospitals and hospices. This finding is consistent with that of an earlier Hong Kong study,(10) in which older age was an independent predictor for preferring nursing homes as the place of death. It is also supported by a British qualitative study(11) that evaluated patients’ concerns and worries about dying at home. This finding highlights the necessity to avoid the assumption that institutional death cannot be a ‘good death’ and the important role of advanced care planning to ascertain a patient’s preference.
In this study, when participants were asked what they preferred for themselves if they were uncommunicative and completely dependent in self-care, most healthcare professionals chose less aggressive treatment; that is, doctors and nurses were less likely to choose CPR and intubation compared to patients and relatives. This finding is similar to the previous literature, which reported that doctors and nurses predominantly wished to forgo high-intensity treatment or resuscitation and opted for comfort care at end-of-life.(12-15) This finding also explained the correlation in the present study between age and preference for CPR and symptom relief treatment, as the doctors and nurses in this study were generally younger than the patients and relatives. The discrepancy could be due to the fact that doctors and nurses may have realised, through exposure, that aggressive treatment does not always change the ultimate outcome for a function-impaired patient and only results in more suffering instead of benefits. However, the concept of medical futility is hard to accept for non-medical personnel, who have little exposure, knowledge or experience with these life-sustaining measures. Furthermore, physicians’ discomfort or reluctance could have resulted in their failure to help patients in advance care planning, as well as lost opportunities for patients to gain a clearer understanding of the risks and benefits of end-of-life care options. Lastly, the participants in the doctor and nurse groups had at least one tertiary degree in healthcare, suggesting that medical knowledge could also influence an individual’s preferences regarding end-of-life care.
When participants were asked to decide on behalf of their loved ones, the doctor, nurse and relative groups surprisingly preferred nasogastric tube feeding for their loved ones, but not for themselves. This may be due to a prevailing cultural belief that feeding is an emotional issue for family members, who worry about their loved one suffering from thirst or hunger. Feeding an elder is seen as the duty and obligation of adult children and as an act of filial piety in Singaporean culture. Therefore, poor oral feeding may be associated with the starvation or neglect of a loved one. The relative and nurse groups also preferred intubation and antibiotics for loved ones in comparison to themselves. This decision may have helped them feel satisfied with having tried their best on someone’s behalf. The relative and nurse groups could also be acting out of fear of the guilt, regret or sense of negligence at the untimely death of the loved one because of their decision not to treat.
Although relatives’ decisions for their loved ones were very different from patients preferences about end-of-life care options for themselves, most patients preferred to nominate relatives as their surrogate decision-makers. The present study indicates that decisions made by the family surrogates may not reliably represent the patient’s preferences and wishes. Consequently, patients who cannot participate in decision-making are most at risk of receiving care inconsistent with their personal preferences. This finding affirms the importance of early and effective patient-surrogate communication on end-of-life care while the patient is still mentally capable of making decisions for themselves. The discrepancy in attitudes between healthcare professionals (doctors and nurses) and healthcare recipients (patients and relatives) also underlines the importance of healthcare professionals’ participation in communication, preferably at initial stages of a patient’s terminal disease and impaired function. Effective communication is difficult and requires that the healthcare team have a high level of comfort in discussing end-of-life care and death, especially as death is still a taboo subject in Singapore. To help individuals ensure that the care they receive during times of decisional incapacity is guided by their preferences, greater resources are required for public education, development of end-of-life care and services, as well as increasing the capability of healthcare professionals. There should be open discussion and an exchange of ideas to improve the existing healthcare system, emphasising the development of new ideas and new policies to guarantee the fairness of access to good healthcare, and seamless and appropriate care for patients and their families. A plan for national advanced care must be drawn up to determine the choices or desires of every patient and to ensure that these wishes are fulfilled. This will also relieve the caregivers (i.e. usually relatives) from the burden of having to make the decision on their behalf, which would reduce unnecessary consumption of healthcare services as well as respect the patient’s wishes and dignity.
There were limitations to this study as our findings may not be applicable to other settings or a younger population. This could be because a majority of the healthcare professionals specialised in geriatric medicine, with considerable exposure to end-of-life care, and the majority of the patients surveyed were elderly (65 years of age and above). Furthermore, the survey responses of patients were not analysed together with those of their own relatives, although a direct comparison between patients’ and their respective caregivers/relative’s wishes for end-of-life care would be ideal. In addition, only completed survey forms were included in this study. In order to ensure the accuracy of survey answers, patients whose cognitive capability was impaired by moderate dementia or worse were also excluded.
CONCLUSION
It is crucial that every patient’s end-of-life care decision is appropriately made. This study surfaces differences in the attitudes toward end-of-life care among patients, relatives and healthcare professionals such as doctors and nurses. We propose early and open communication among patients, their family and healthcare professionals to close the gap between their expectations and ensure that the patient’s autonomy and best interests are served at all times, especially at the end of their life, when their voices may be inaudible.


