14-year-old Melissa visited your clinic with her mother for concerns of secondary amenorrhoea of six months. She did not have any headaches or visual disturbances and was not on any long-term medication. She also had dry skin and constipation. Her mother mentioned that Melissa had lost 8 kg of body weight in the past six months, leading to her current weight of 38 kg, citing school-related stress as a major factor. Melissa skipped meals in school and was unable to eat more than half a portion at dinner as she felt bloated and full easily, and got angry when her mother encouraged her to eat more. Her mother had noticed that she was more withdrawn and irritable recently. On examination, Melissa was 165 cm tall and weighed 38 kg. Her blood pressure was 92/58 mmHg, and her heart rate was 56 beats/min. You suspected the possibility of an eating disorder and decided to seek a more detailed history and targeted physical examination.
WHAT IS AN EATING DISORDER?
Eating disorders are complex illnesses related to abnormal eating behaviours that can affect the biopsychosocial health and functioning of the affected individuals. Most eating disorders involve an obsessive focus on body image, body weight and food, leading to dangerous eating patterns that have deleterious effects on the young person’s nutrition, growth and development. Other types of eating disorders may not necessarily centre around body image concerns, but can also involve behaviours that impede weight gain, or involve a compulsive drive to pursue health and fitness.
The more common type of eating disorders that may present to a general practitioner or paediatrician include anorexia nervosa (AN) and bulimia nervosa (BN), both of which can lead to medical complications associated with malnutrition or purging. Features of AN include a significant restriction of intake relative to daily requirements and presence of body image disturbance with undue influence of body weight/shape on self-evaluation. BN similarly stems from obsessive concerns over body shape and weight but is distinguished from AN by the presence of binge eating and recurrent compensatory behaviour to prevent weight gain, such as purging and the use of laxatives or diuretics.(1) It is important to note that individuals with eating disorders do not necessarily have a low weight or body mass index (BMI).
While it is developmentally normal for adolescents to develop an increased interest in their appearance and body image, significant weight loss or overly restrictive dietary habits are not a normal phase of adolescence, and adolescents exhibiting such behaviour should be evaluated for serious conditions such as an eating disorder.
In our local context, many patients with eating disorders may not present with concerns of weight loss or specifically for evaluation of an eating disorder, but may instead present with physical manifestations and complications of malnutrition such as bloating, abdominal pain, early satiety, constipation, giddiness, secondary amenorrhoea and low mood.(2)
HOW COMMON IS THIS IN MY PRACTICE?
Eating disorders commonly develop in adolescence, with conditions such as AN and BN having an average age of onset of 14 years.(2) They present more commonly in females, but also occur in the male population. Studies conducted worldwide have estimated the lifetime prevalence of AN to be between 0.5% and 2.0%, and that of BN to be between 0.9% and 3.0%. A Singapore-based study by Ho et al(3) found that 7.4% of females (aged 12–26 years) are at risk of developing an eating disorder.
Eating disorders are serious illnesses and have the highest mortality rate among all psychiatric disorders, with mortality stemming from both the physical and psychiatric complications.(4) Eating disorders are underdiagnosed and undertreated, as most affected patients have poor insight and deny the severity of their illness.(5) The primary care physician is uniquely positioned to detect the warning signs of early eating disorders, as adolescents commonly present to primary care for concerns or complications resulting from eating disorders.(6) Early identification and diagnosis of eating disorders by primary care physicians is critical, as timely intervention is associated with a higher likelihood of successful treatment. Studies have shown that early intervention is associated with higher rates of recovery.(5,7)
Studies have found that female gender, concurrent psychiatric disorders such as mood and anxiety disorders, and premorbid perfectionistic personality traits are risk factors for developing eating disorders. A family history of a close relative with an eating disorder or psychiatric illness has also been found to be associated with a higher risk of developing an eating disorder. It is important to note that eating disorders can also occur in individuals with no significant risk factors and in males. In males, body image concerns may involve fitness, muscularity, and engaging in muscle-enhancing behaviours such as eating more or differently or taking supplements to build muscles.(8,9)
WHAT CAN I DO IN MY PRACTICE?
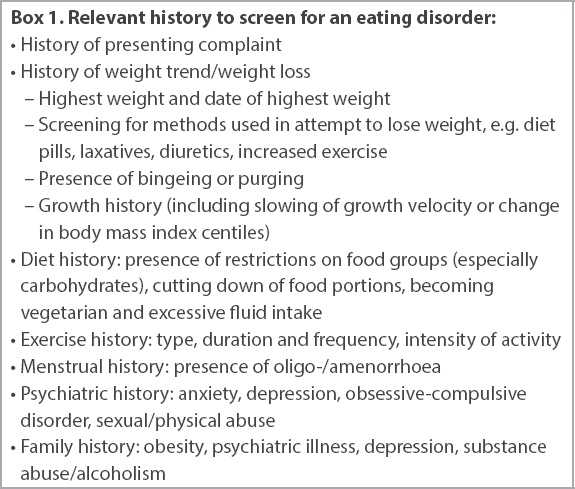
When symptoms of weight loss, disordered eating or medical complications of malnutrition have been identified, a more detailed assessment should follow. History should be obtained in a non-judgemental, empathetic manner to understand the adolescent’s experience, and to determine whether he/she may require further evaluation by an eating disorder specialist. A history of weight loss should be explored, focusing on intentionality and the ways in which the weight loss was achieved (e.g. by use of laxatives or purging). Commonly, adolescents may report a strong interest in healthy eating and behaviours as opposed to body image, but excessive exercise, change in eating behaviours, restrictive eating patterns and the presence of binge-purge activity may still point towards an underlying eating disorder (
Box 1
Relevant history to screen for an eating disorder:
Box 2
Possible physical examination findings of patients with eating disorders:
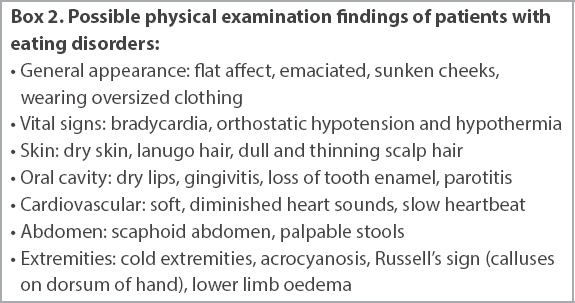
Many patients with eating disorders often present with non-specific symptoms such as headaches or complications of malnutrition. Complications of malnutrition include abdominal discomfort and bloating, alopecia, dry skin, easy bruising, constipation, dizziness, recurrent headaches, secondary amenorrhoea or persistent primary amenorrhoea, or other disruptions of normal pubertal events. It is important to consider other medical conditions (e.g. gastrointestinal or autoimmune conditions) that can lead to weight loss through careful history-taking and targeted physical examination. Diagnosing eating disorders in primary care practice can, thus, be challenging and some common pitfalls may be encountered in clinical practice.
- Owing to the rapid increase in height during the pubertal growth spurt period, absolute weight loss may not appear drastic, although there is a significant change in BMI. It can often be challenging to establish a weight trajectory, as adolescents may not have a history of documented weights.
- Adolescents may not always express body image issues or a fear of weight gain, as their underlying motivations for the weight loss may be different, and some younger adolescents may not be developmentally able to express these concerns. They may present with non-specific symptoms or complications of malnutrition.
- Some younger adolescents may not have achieved menarche owing to their age; hence, secondary amenorrhoea may not be present.
- Dieting behaviours and body image concerns are highly prevalent in adolescents and may be dismissed as a normal phase of adolescent development.
- Restrictive eating disorders occur not only in thin or underweight adolescents but also in patients with BMIs in the normal or overweight range.(4) Despite having a normal or high BMI at presentation, they are similarly at risk of medical complications from rapid weight loss.(10) In fact, adolescents with obesity are at an increased risk of eating disorders.
- While eating disorders are more common in females, males can also be affected, with more muscularity-oriented eating disorder symptoms.(8)
Management of patients with eating disorders
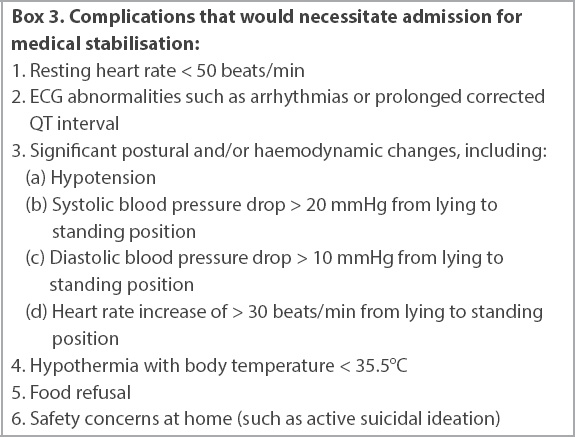
In the primary care setting, the physician’s priority is to ensure that the patient is medically stable and does not have significant complications from eating disorders that necessitate an urgent referral to the emergency department of a tertiary medical centre (
Box 3
Complications that would necessitate admission for medical stabilisation:
For medically stable patients, early referral to an eating disorder specialist is warranted. A multidisciplinary team will be involved in the care of the child, and commonly includes paediatricians, specialist nurses, psychologists, psychiatrists, dietitians and social workers.
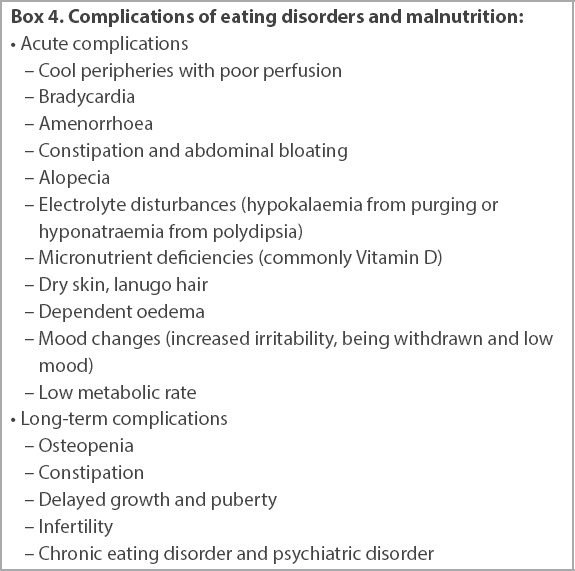
Upon referral to an eating disorder specialist, the adolescent will be assessed for medical mimics and evaluated for complications of eating disorder (
Box 4
Complications of eating disorders and malnutrition:
Outpatient treatment goals are medical and psychological recovery from the eating disorder. Family-based therapy (FBT), also known as the Maudsley approach, is the first-line, evidence-based psychological treatment used in most tertiary care centres for AN and has been shown to have the best treatment outcomes, including protection against relapse. FBT adopts a non-blaming approach to eating disorders, and focuses on empowering and engaging parents in the refeeding process. The FBT process emphasises early restoration of weight and nutrition, and resumption of regular meal patterns and eating habits.(5) In our local study, patients with AN treated with FBT had faster and improved rates of weight restoration compared to patients treated without FBT.(11)
While awaiting specialist care, the family physician can inform both the adolescent and the family about the complications of restrictive eating and malnutrition, and start them on eating regular-sized meals more frequently. It is important to reinforce that neither the parent nor the teen caused the development of an eating disorder. Frequent monitoring of the adolescent’s physical health is also important, as a medical instability can occur while awaiting the involvement of a specialist team in cases of rapid weight loss and food restriction. Important early messages for families when there are concerns about restrictive eating disorders are: (a) encouraging the family to provide and support three main meals and three snacks a day; (b) excusing the adolescent from all co-curricular activities, physical education classes and excessive physical activity; and (c) seeking timely consultation with an eating disorder specialist or team.
TAKE HOME MESSAGES
-
Eating disorders are challenging to diagnose and the common pitfalls should be noted. They should be diagnosed early in the disease process to reduce morbidity and improve chances of recovery.
-
A targeted history and physical examination while looking out for signs, symptoms and complications of eating disorder are important for early detection of eating disorders.
-
Primary care physicians should be familiar with medical complications of eating disorders and assessment of medical stability.
-
Management of an eating disorder is multidisciplinary, involving doctors, nurses, dietitians and social workers or psychologists. Referral to specialist care is indicated for adolescent patients suspected to have an eating disorder.
On further history-taking, Melissa shared that she had intentionally been trying to lose weight by counting calories, restricting her diet and exercising more. There was no purging or laxative use. You spoke to Melissa and her mother about your concerns regarding an eating disorder, informed them about the complications, and referred Melissa to an eating disorder programme in a tertiary centre. In the meantime, Melissa and her mother agreed to work on increasing her meal portion sizes. You wrote a memo to excuse her from physical education and co-curricular activities, and arranged to see her again in a week to review her weight and vitals. Melissa was subsequently seen by a specialist and diagnosed with anorexia nervosa. She started family-based therapy and experienced good weight gain and restoration of her menses.
Supplementary Material
SMJ-63-298.pdf


