Abstract
INTRODUCTION
This study aimed to assess the effectiveness of the use of a cardiopulmonary patient simulator in the teaching of second-year medical students. Effectiveness was measured in terms of the extent of knowledge retention and students’ ability to apply the skills learned in subsequent real-life patient contact.
METHODS
In this study, ten third-year medical students who had previously undergone simulator training as part of their second-year curriculum underwent an objective structured clinical examination (OSCE) and a multiple-choice question (MCQ) test to assess their ability to apply the knowledge gained during the simulator training when dealing with real patients. The performance of this group of students was compared with that of a group of ten fourth-year medical students who did not undergo simulation training.
RESULTS
Although the third-year medical students performed well in the OSCE, they were outperformed by the group of fourth-year medical students, who had an extra year of clinical exposure. The MCQ scores of the two groups of students were similar. Post-simulation training survey revealed that students were generally in favour of incorporating cardiopulmonary simulator training in the preclinical curriculum.
CONCLUSION
Cardiopulmonary simulator training is a useful tool for the education of preclinical medical students. It aids the translation of preclinical knowledge into real-life clinical skills.
INTRODUCTION
The use of simulation in education has been increasingly prevalent in recent years and medical education is no exception to this phenomenon. While experiential-based learning is highly valued in medical education,(1,2) it is limited by patient safety considerations(3-7) and the relatively low access medical students have to patients. The use of simulation training in clinical education may circumvent such constraints. In fact, high-fidelity medical simulations have been shown to be educationally effective, and simulation-based education has been shown to complement traditional bedside teaching.(8) Most studies report that medical students who underwent simulation training had improved test scores in assessments that measure clinical skill and knowledge.(9-14) Furthermore, simulation training may be more practical in certain situations; for example, during an epidemic, students may not be allowed to practise physical examination of patients in wards. One study performed during the severe acute respiratory syndrome epidemic in 2003 explored the utility of teaching cardiac auscultation without patient contact.(15) For that study, patients with echocardiographically proven heart disease had their heart sounds recorded on electronic stethoscopes. After these recorded sounds were validated, they were used to teach students during simulated bedside sessions. The objective outcome measures and subjective feedback in that study demonstrated that the method was effective and well-received by the students.(15) However, there is still a lack of conclusive research on the cost-benefit factors of the use of simulation in education, and a lack of evidence on the real impact simulation has on actual patient care.(16)
The simulator employed in the teaching of the cardiovascular system is Harvey® The Cardiopulmonary Patient Simulator (Laerdal Medical, Stavanger, Norway). The simulator is a full-size manikin that is able to realistically simulate more than 30 cardiac conditions (through various clinical signs such as heart sounds, murmurs, jugular venous pulsation, nature of apex beat and breath sounds) at the touch of a button. It can be structured to teach students not only common and less complex conditions, but also rare and complex diseases. The main goal of the learning activity using the simulator is for students to understand the functionality of the cardiovascular system under normal physiological conditions and to appreciate how it is affected in various disease processes. The Harvey simulator has been shown to be effective in enabling students to achieve a reasonable level of competency in the skills taught.(17) As such, it has been accredited and recommended for medical education by many institutions worldwide. In fact, the British Heart Foundation purchased a Harvey simulator for each medical school in the United Kingdom.(18)
The undergraduate curriculum of the Yong Loo Lin School of Medicine, National University of Singapore, Singapore, was revised in 2008 to integrate the content covered and increase the relevance of the basic science curriculum, so as to better equip students for the clinical phases of medical school. A key feature of the revised curriculum is the incorporation of simulation in the systems-based preclinical modules. The cardiovascular system module is one such example. The use of the Harvey simulator was incorporated into the teaching-learning schedule of each group of medical students, so as to expose them to core must-know conditions in cardiovascular diseases through hands-on practice sessions. The Harvey simulator allows students to practise examination of a ‘patient’ with varied signs, some of which may be rare in clinical practice. In other words, it may take many weeks or months for students to encounter all the same signs (i.e. to gain the same experience via simulation training) through the examination of real patients in normal clinical practice.
The present study was designed to evaluate the effectiveness of the revised curriculum with Harvey in enhancing medical students’ knowledge retention and their ability to apply the knowledge and skills acquired (during the simulation training) to actual clinical cases. The study also included a survey of the students’ perception of their level of confidence in applying what was learned to their future clinical clerkships.
METHODS
A total of ten students in their third year of medical study were recruited to undergo an objective structured clinical examination (OSCE) and a multiple-choice question (MCQ) test. These students had undergone the revised curriculum that included Harvey simulation and completed two years of basic science training, but have yet to undergo internal medicine or paediatric rotations. The results of the OSCE and MCQ test were examined, and a post-examination survey (see
All of the ten students had attended two 3-hour, hands-on simulation training sessions when they were second-year medical students. In the first session (an introductory session), the students familiarised themselves with the simulator. Facilitators guided the students through general scenarios and discussions about the physiological and anatomical bases of relevant clinical signs. Students were given the opportunity to go through the clinical signs repeatedly until they were familiar with them. The second session was a revision of the murmurs and clinical scenarios. After these two short sessions with the simulator, the students were not exposed to cardiology or internal medicine rotations for about a year, up to the time they participated in the present study. Another ten students who were in their fourth year of medical study were recruited to undergo the same OSCE and MCQ test without a post-test survey.
Both groups of students were required to undergo five OSCE stations that examined core clinical competencies in cardiology. At each OSCE station, students were required to examine a real patient with one of the following cardiac conditions: aortic stenosis, mitral stenosis, mitral regurgitation, mitral valve prolapse and a prosthetic valve. The students presented their findings to an examiner, who then graded them based on an objective marking scheme comprising the following components: (a) student’s general approach and rapport with the patient; (b) student’s examination technique; and (c) student’s ability to pick up on clinical signs and carry out a short discussion of the case. This is similar to the validated assessment template that the Yong Loo Lin School of Medicine uses for its professional examinations. The OSCE examiners were practicing cardiologists who had examined and verified the clinical findings in the patient. Each student was tested on the same patient and graded by the same examiner, which translates into higher consistency and greater objectivity in the assessment. Upon completion of the OSCE, the third-year students were asked to complete a survey on the utility and limitations of the Harvey simulation sessions.
The MCQ test comprised 32 questions that primarily examined the students’ understanding of important physical signs, including pathophysiology in cardiology and its relation to various conditions. The questions were in the ‘best answer out of four choices’ format and the students were allocated an hour to complete the test. There was no negative marking.
RESULTS
The OSCE stations were scored according to the following four categories: (a) general approach; (b) examination technique; (c) signs; and (d) synthesis. The third-year medical students, who were examining real patients for the first time, did reasonably well in the OSCE. The OSCE and MCQ test results of the third- and fourth-year medical students are shown in
Table I
Comparison of performances between the third- and fourth-year medical students in the objective structured clinical examination (OSCE) stations and multiple-choice question (MCQ) test.
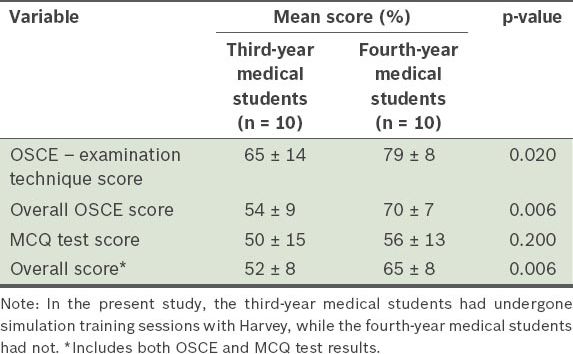
For the MCQ test, the mean scores of the third- and fourth-year medical students were 50% ± 15% and 56% ± 13%, respectively. However, this difference was not found to be statistically significant (p = 0.20). Combining the OSCE results with the MCQ test results, the overall mean scores for the third- and fourth-year medical students were 52% ± 8% and 65% ± 8%, respectively.
Based on the post-examination survey conducted on the third-year medical students who participated in the simulation sessions, the students generally felt that the sessions provided them with greater opportunity for practice and boosted their confidence for clinical rotations. Although there were drawbacks to the simulation sessions such as its limited duration, the large class size and the lack of variability in the severity of clinical signs (which is normally seen in real patients), all the students had positive comments on it.
DISCUSSION
The present study looked at whether a simulation module would help medical students in their clinical rotations and subsequent learning in the clinical years. Bearing in mind that in this study, the OSCE represented the third-year medical students’ first contact with real patients who had cardiovascular signs, the students did reasonably well with regard to their examination technique. This shows that training with the Harvey simulator in the preclinical years helps students acquire foundational skills in cardiology and medicine, and that this form of learning is a useful adjunct in medical education.
Comparing the OSCE results of the third-year medical students with that of the fourth-year medical students, we found that most of the third-year medical students managed to score well in the examination technique category, which is the category that Harvey simulation specifically trains for. The third-year medical students scored reasonably well despite not having gone through any formal clinical rotation in internal medicine. They relied mainly on the skills that they had picked up during the simulation training. Compared to the third-year medical students, the fourth-year medical students scored better in the skill sets tested during the OSCE and achieved better overall OSCE scores. This is not unexpected in light of the extra year of clinical exposure that the fourth-year medical students had gone through. Although the fourth-year medical students had varied degrees of exposure to cardiac cases during their clinical postings in various hospitals, the types of patients that were tested in the OSCE were core clinical cases, as indicated in the undergraduate curriculum. During the course of their posting, the fourth-year medical students would have had sufficient opportunities to see patients with the conditions tested in the OSCE, thus enabling them to do well in the OSCE stations.
It was interesting to note that although the present study examined what third-year medical students had learned in their second year, they appeared to be able to retain what they had learned even after a year and were able to perform reasonably well in the OSCE. This is despite the students having undergone only two sessions of simulation teaching for the cardiovascular system.
In the present study, the scores for the third- and fourth-year medical students were comparable in some instances. First, there was no significant difference in the MCQ test scores between the two groups. Also, in the part of the OSCE that focused on the physiology and pathology of cardiovascular physical examination findings, the medical students in both groups obtained similar scores. This could be due to the fact that during their second year of medical training, the medical students had undergone a Harvey simulation course, in which they were taught these topics. Therefore, it is plausible that that the Harvey simulation sessions, together with the integration of their preclinical years with the clinical curriculum, had benefitted the students in applying what they had learnt in preclinical modules to clinical practice.
In the post-examination survey, the third-year medical students were asked about the difficulties faced during the transition from preclinical years to clinical years. Many stated that they lacked confidence in approaching patients and had difficulty remembering the examination steps. Many also mentioned that there was a lack of patients willing to be examined by medical students. However, with the use of Harvey simulation, medical students are given the opportunity to hone their examination technique before approaching real patients. This may help to boost their confidence during clinical rotations. The use of Harvey simulation also alleviates the problem of patient fatigue, as medical students are given the chance to practice on simulators and thus do not require patient contact for every physical examination practice. Other concerns raised by the medical students in the post-examination survey were the short duration and large class size of the simulation sessions. It is advisable to take these points into consideration in future simulation training sessions, so as to optimise the learning of each medical student.
The present study was not without limitations. One obvious limitation is the small number of medical students in each of the groups analysed. This was the case because the study was planned as a pilot study. However, despite the small numbers, significant differences were still observed.
Several studies have shown that deliberate practice leads to expert performance.(1,2) The ability to accurately diagnose a condition hinges on the rarity of the disease and the duration of deliberate practice in appropriate clinical settings. While the use of the Harvey simulator is not meant to replace traditional bedside teaching, it is a potentially useful adjunct in medical education, as it allows hands-on practice in a risk-free environment, boosting students’ confidence in their subsequent interaction with real patients. The use of the Harvey simulator is especially useful in helping medical students develop the right examination technique for cardiovascular examination. Lengthening the duration of the Harvey simulation sessions and decreasing the class size may increase the learning value of the lessons.
SMJ-56-102-appendix.pdf
ACKNOWLEDGEMENTS
We acknowledge Dr Dujeepa D Samarasekera for his advice and help in the project and in the writing of this paper. We thank Ms Lee Ai Lian and Ms Hazel Phua for their help with the logistics of this study. We also acknowledge Dr Lim Shir Lynn, Dr Low Ting Ting, Dr Kyu Kyu and Dr Charles Ng for their help in conducting the study.


