Abstract
Plantar fasciitis is a very common cause of inferior heel pain that can be triggered and aggravated by prolonged standing, walking, running and obesity, among other factors. Treatments are largely noninvasive and efficacious. Supportive treatments, including the plantar fascia-specific stretch, calf stretching, appropriate orthotics and night dorsiflexion splinting, can alleviate plantar fascia pain. While local injections of corticosteroids can help with pain relief, the effects are short-lived and must be weighed against the risk of fat pad atrophy and plantar fascia rupture. Ultrasonography-guided focal extracorporeal shock wave therapy is useful for patients with chronic plantar fasciitis and referrals for this treatment can be made in recalcitrant cases. Activity modification to decrease cyclical repetitive loading of the plantar fascia should be advised during the treatment phase regardless of the chosen treatment modality.
Albert limped into your consultation room complaining about the right foot pain he had been having for the past three weeks, which was especially excruciating upon his first few steps from his bed. He related that the pain began a week after he started preparing for a half marathon as part of his company’s ‘Get healthy’ pledge. He had joined the running interest group in their daily long runs, but dropped out after only one week due to the right foot pain and occasional painful cramps in his calf muscles at night. Although Albert has taken diclofenac tablets daily over the past week, the pain has persisted..
WHAT IS PLANTAR FASCIITIS?
Plantar fasciitis is the most common cause of plantar heel pain, with an incidence of one million patient visits per year in the United States of America.(1) Even so, the exact histopathology of plantar fasciitis is not fully understood. It is currently thought to be secondary to myxoid degeneration, microtears within the plantar fascia, collagen necrosis and angiofibroblastic hyperplasia of the plantar aponeurosis, and not due to an inflammatory process.(2)
Presentation
The patient usually presents with gradual onset of pain over the medial side of the plantar heel that is most noticeable when taking the first few steps in the morning. The pain may get better after a short period of walking, but returns when performing activities that involve prolonged weight-bearing, such as standing, walking or running. The patient may also complain that heel pain worsens after repeat weight-bearing following a period of rest, such as standing after a period of sitting at a desk.
Risk factors
The plantar fascia runs from the calcaneus to the toes; most of the load falls on its medial edge, from the medial calcaneal process to the first toe. As the plantar fascia helps to hold up the medial arch of the foot, any load on the medial arch (e.g. on weight-bearing) stretches the plantar fascia. Most lesions occur at the origin of the fascia, the medial calcaneal process. The plantar fascia is also loaded via the windlass mechanism of the foot when the big toe is dorsiflexed, such as in forefoot running.
Any factor that mechanically loads the plantar fascia can be considered a risk factor for plantar fasciitis. Risk factors can be divided into intrinsic and extrinsic factors. Intrinsic factors relating to the patient include obesity, pes planus, pes cavus, reduced range of ankle dorsiflexion and tight calf muscles.(3) Extrinsic factors, relating to the environment and training, include running on hard surfaces, walking barefoot, a sudden increase in running intensity and/or volume, and prolonged walking/standing.(3)
WHAT CAN I DO IN MY PRACTICE?
Imaging
Radiography has limited value in the diagnosis of plantar fasciitis. However, a lateral weight-bearing view of the foot may be helpful in excluding differentials such as acute calcaneal fracture, or Sever’s disease (calcaneal apophysitis) in younger patients. 50% of patients with plantar heel pain may have heel spurs, but the relationship to subcalcaneal pain has not been established.(4,5) Heel spurs are now thought to be a result of traction forces on the plantar fascia origin rather than the cause of plantar fasciitis.
Musculoskeletal ultrasonography is a very useful and reliable tool in diagnosing plantar fasciitis, as it is a well-tolerated, noninvasive imaging modality with no ionising radiation. According to published normative values, plantar fascia thickness in asymptomatic healthy adults ranges from 3.3 ± 0.3 mm to 3.9 ± 0.5 mm; a thickness greater than 4.0 mm is considered abnormal.(6-10) Apart from quantifying and thereby monitoring the severity of the plantar fasciitis, ultrasonography can conclusively exclude a differential diagnosis such as plantar fascia fibromatosis, which appears as a fusiform swelling distal to the plantar fascia origin, and heel pad contusions, which are superficial to the plantar fascia.
Treatment
Treatment is largely nonoperative, with 90%–95% of patients experiencing resolution of symptoms within 12–18 months.
Activity modification
Modification of activities should be advised, while those that involve repetitive impact, such as running (even on a treadmill), should be avoided during the treatment phase. Patients can continue performing non-weight-bearing activities such as cycling, swimming and rowing to maintain their cardiovascular fitness while minimising cyclic loading. A gradual return to activity may be allowed after the patient is asymptomatic for 4–6 weeks and no longer has localised tenderness over the plantar fascia.
Plantar fascia stretch and ice massage
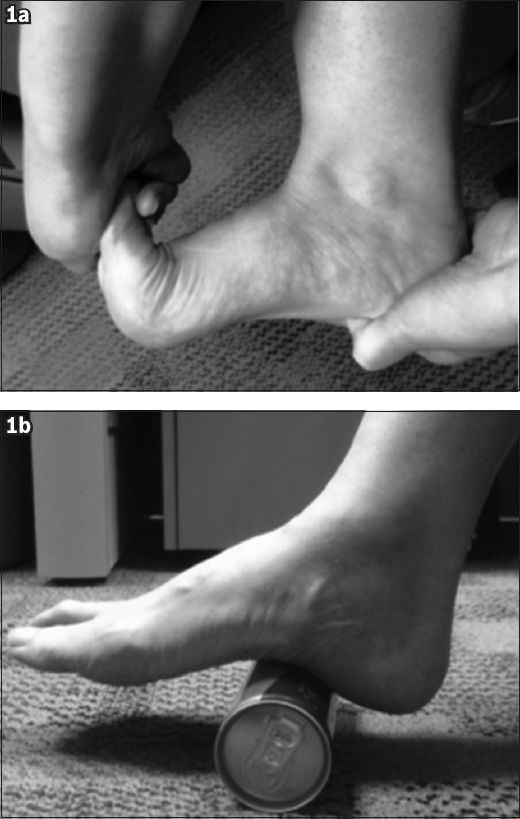
Plantar fascia and calf stretches are inexpensive and easy to learn. The plantar fascia-specific stretch has been shown to be more efficacious than the isolated Achilles stretching programme.(11) The plantar fascia-specific stretch is performed by dorsiflexing the toes with one hand (taking advantage of the windlass mechanism) and palpating the plantar fascia with the other hand to ensure that it is taut (
Fig. 1
Photographs show (a) the plantar fascia-specific stretch, and (b) the ice massage method, which involves rolling a frozen can under the foot.
Night splints
The use of night dorsiflexion splints can also help with plantar fasciitis, especially pain that is worse during the first few steps in the morning. Night splints have produced highly positive outcomes such as resolution of symptoms within 12 weeks of use. The patient may see improvement as early as after four weeks of use.(12)
Orthotics
To reduce loading of the plantar fascia on weight-bearing, orthotics should help to hold up the medial arch of the foot without placing any direct pressure on the plantar fascia. Additionally, to reduce the direct pressure of the ground on plantar fascia swelling, an aperture can be incorporated into the orthotic such that the swelling sits in the aperture. For athletic individuals, semi-rigid orthotics are the most practical solution, and it is helpful for physicians to specify ‘semi-rigid orthotics with plantar fascia accommodation and aperture’ when prescribing orthotics to be fabricated by a podiatrist. The use of orthotics, including heel cups and plantar fascia support insoles, was found to be effective in alleviating pain from plantar fasciitis. In addition, it was shown that prefabricated insoles were not inferior to custom-made ones, giving patients without true biomechanical abnormalities, such as pes planus/cavus, a more economical option.(13,14) However, as prefabricated insoles come in a myriad of designs, physicians should exercise caution when making generalisations.
Analgesia
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) to treat plantar fasciitis is a widespread practice that has been called into question, as plantar fasciitis is not an inflammatory process. This is supported by a recent study showing no significant difference in pain and disability scores in patients who were given NSAIDs compared to those who received a placebo.(15) However, when combined with other treatment modalities, NSAIDs or simple analgesics may help to provide short-term pain relief.(14)
Steroid injection
Localised steroid injections into the plantar fascia have been shown to provide effective short-term relief of plantar fascia pain for up to three months.(16) There is, however, increased risk of plantar fat pad atrophy and plantar fascia rupture with repeated corticosteroid injections,(17) and thus, repeated injections should be avoided if possible.(18)
Platelet-rich plasma injection
Localised platelet-rich plasma injections have shown much promise and appear to be safe.(19) However, this modality is currently not approved by the Ministry of Health, Singapore, for the treatment of plantar fasciitis.
Focal extracorporeal shockwave therapy
Patients with recalcitrant plantar fascia pain can be referred to hospitals that offer ultrasonography-guided focal extracorporeal shockwave therapy (fESWT) as part of their sports medicine service. This treatment has been shown to be efficacious for patients with chronic plantar fasciitis that did not respond well to conservative treatment.(20,21) fESWT is a noninvasive procedure that takes about ten minutes per treatment; the patient usually requires two treatments spaced one week apart for optimal efficacy.(22,23)
Operative treatment
If the patient continues to have moderate to severe symptoms that do not respond to nonoperative treatment for more than 6–12 months, referral to an orthopaedic surgeon for operative treatment may be required.
Albert dropped by your clinic two weeks later to thank you for treating his pain with only the calf and plantar fascia-specific stretch you taught him. He had since revised his health pledge to include a regular exercise programme that combines stationary cycling and a slow jog. He will gradually work toward 150 minutes of moderate exercise a week and will postpone his half marathon pledge for another year.
TAKE HOME MESSAGES
-
Plantar fasciitis is a common cause of plantar heel pain that can be treated effectively in the outpatient setting.
-
Prolonged standing, decreased range of ankle dorsiflexion, an intense running regime and obesity are all risk factors for plantar fasciitis.
-
A multipronged approach aimed at reducing the load on the plantar fascia is most effective.
-
Activity modification, plantar fascia-specific stretches, calf stretching, orthotics (including cushioned heel cups) and night dorsiflexion splinting can help alleviate symptoms.
-
NSAIDs have limited efficacy for plantar fasciitis.
-
The pain-relieving effects of localised injection of corticosteroids are short-term; its use must also be weighed against the potential side effects of fat pad atrophy and plantar fascia rupture.
-
In moderate to severe cases, ultrasonography-guided fESWT is indicated to supplement the supportive measures mentioned above.
-
Changes in a patient’s training regime, including reduction of mileage and cross training with low-impact activities such as elliptical machine or stationary cycling, are advisable until the symptoms resolve.
-
Referral for operative treatment may be required in patients who continue to have moderate to severe symptoms that do not respond to nonoperative treatments after 6–12 months.
SMJ-57-171.pdf


