Abstract
INTRODUCTION
Physiotherapy is an important part of rehabilitation following arthroplasty, but the impact of preoperative physiotherapy on functional outcomes is still being studied. This randomised controlled trial evaluated the effect of preoperative physiotherapy on the short-term functional outcomes of primary total knee arthroplasty (TKA).
METHODS
50 patients with primary knee osteoarthritis who underwent unilateral primary TKA were randomised into two groups: the physiotherapy group (n = 24), whose patients performed physical exercises for six weeks immediately prior to surgery, and the nonphysiotherapy group (n = 26). All patients went through a similar physiotherapy regime in the postoperative rehabilitation period. Functional outcome assessment using the algofunctional Knee Injury and Osteoarthritis Outcome Score (KOOS) scale and range of motion (ROM) evaluation was performed preoperatively, and postoperatively at six weeks and three months.
RESULTS
Both groups showed a significant difference in all algofunctional KOOS subscales (p < 0.001). The mean score difference at six weeks and three months was not significant in the sports and recreational activities subscale for both groups (p > 0.05). Significant differences were observed in the time-versus-treatment analysis between groups for the symptoms (p = 0.003) and activities of daily living (p = 0.025) subscales. No significant difference in ROM was found when comparing preoperative measurements and those at three months following surgery, as well as in time-versus-treatment analysis (p = 0.928).
CONCLUSION
Six-week preoperative physiotherapy showed no significant impact on short-term functional outcomes (KOOS subscales) and ROM of the knee following primary TKA.
INTRODUCTION
Physiotherapy has long become the pivotal component of rehabilitation following total joint arthroplasty (TKA) and other orthopaedic procedures. However, limited information is available on the potential role of physiotherapy in preparation for surgery, as previous studies had diverse results.(1-8) Prehabilitation, or the concept of preparing the body prior to a stressful event such as surgery, aims to develop patients’ ability to withstand stress in order to maximise postoperative outcomes. Patients who undergo successful prehabilitation are expected to have shorter recovery times, less dependence on caregivers and faster recovery of preoperative functions.(2)
These positive results may have particular relevance to arthroplasty surgery, as the postoperative status of hip and knee arthroplasty patients is strongly related to preoperative functional status.(1) In a review, preoperative physiotherapy was suggested to have some postoperative benefits for total knee or hip arthroplasty patients; however, the results were inconclusive due to lack of strong research evidence.(3) The findings of another study had uncertain clinical significance and failed to support the routine use of preoperative physical therapy in knee replacement therapy.(4) Results from other studies were inconclusive due to their small sample size and methodological limitations such as the use of less effective exercise intervention.(5-8) This study was designed to evaluate the effect of preoperative physiotherapy on the short-term functional outcomes of primary TKA at three intervals – preoperatively, and postoperatively at six weeks and three months – in the course of treatment.
METHODS
A randomised controlled trial was conducted among patients with primary knee osteoarthritis at the Arthroplasty Clinic of Hospital Universiti Sains Malaysia (HUSM) in Kelantan, Malaysia, from 1 June 2010 to 10 August 2011. Institutional ethical approval was obtained before conducting the study. Patients were eligible to participate if they were (a) above the age of 45 years; (b) lived within a convenient distance of the physiotherapy facility; (c) had been diagnosed with unilateral or bilateral primary knee osteoarthritis; and (d) underwent unilateral TKA at HUSM. Patients with the following conditions were excluded: systemic inflammatory arthritis; degenerative joint diseases involving the hip or ankle joint or spine; medical comorbidities with an inability to tolerate a moderate level of physical exertion; premorbid knee joint stiffness; history of cardiovascular accident; and cognitive, psychological or language impairment. Sample size estimation was performed using PS version 3.0.34 (Dupont and Plummer, Nashville, TN, USA), based on a standard deviation of 11.4 and detectable difference in the population mean of 9.1. The minimum computed sample size was 26, with an estimated dropout rate of 10%. Patient assignment into two groups was randomised according to the week of their surgery; those who were scheduled for surgery on odd and even weeks of the month were assigned to the physiotherapy and nonphysiotherapy groups, respectively. Patient assignment was performed by the primary investigator and this was not made known to the surgeons.
The use of the algofunctional Knee Injury and Osteoarthritis Outcome Score (KOOS) scale required no licence; the questionnaire was downloaded from the website
Preoperative assessment was done on both groups using the algofunctional KOOS and an evaluation of the range of motion (ROM) of the knee. The physiotherapy group performed physical exercises twice weekly over a six-week period immediately prior to surgery. Their physiotherapy regime included stretching, isometric strengthening exercises, mobilising exercises and heat therapy (
Table I
Preoperative physiotherapy regime of the physiotherapy group.
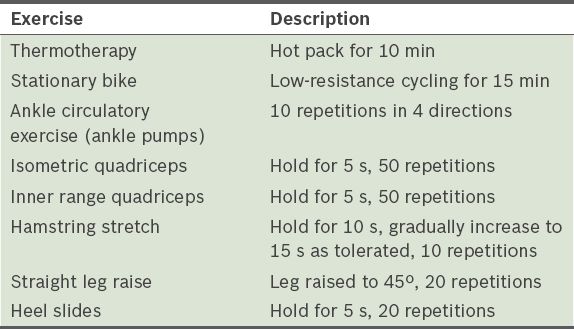
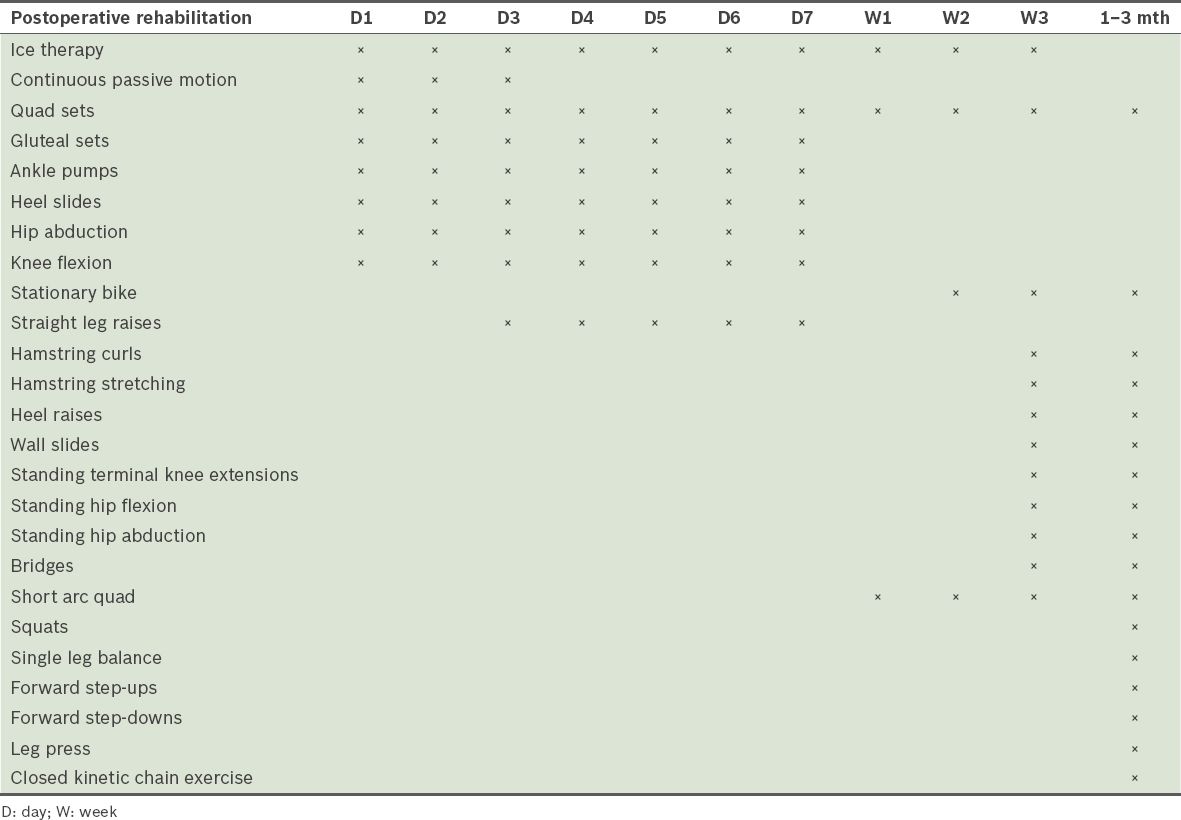
Table II
Postoperative physiotherapy protocol of total knee arthroplasty patients at Hospital Universiti Sains Malaysia.
The primary investigator performed all data collection. Data was analysed using PASW Statistics for Windows version 18.0 (SPSS Inc, Chicago, IL, USA). Numerical variables were presented as mean ± standard deviation, while categorical data was expressed in frequency and percentages. Repeated measures analysis of variance (ANOVA) was used to compare the pre- and postintervention values of all five subscales of KOOS in both groups.
RESULTS
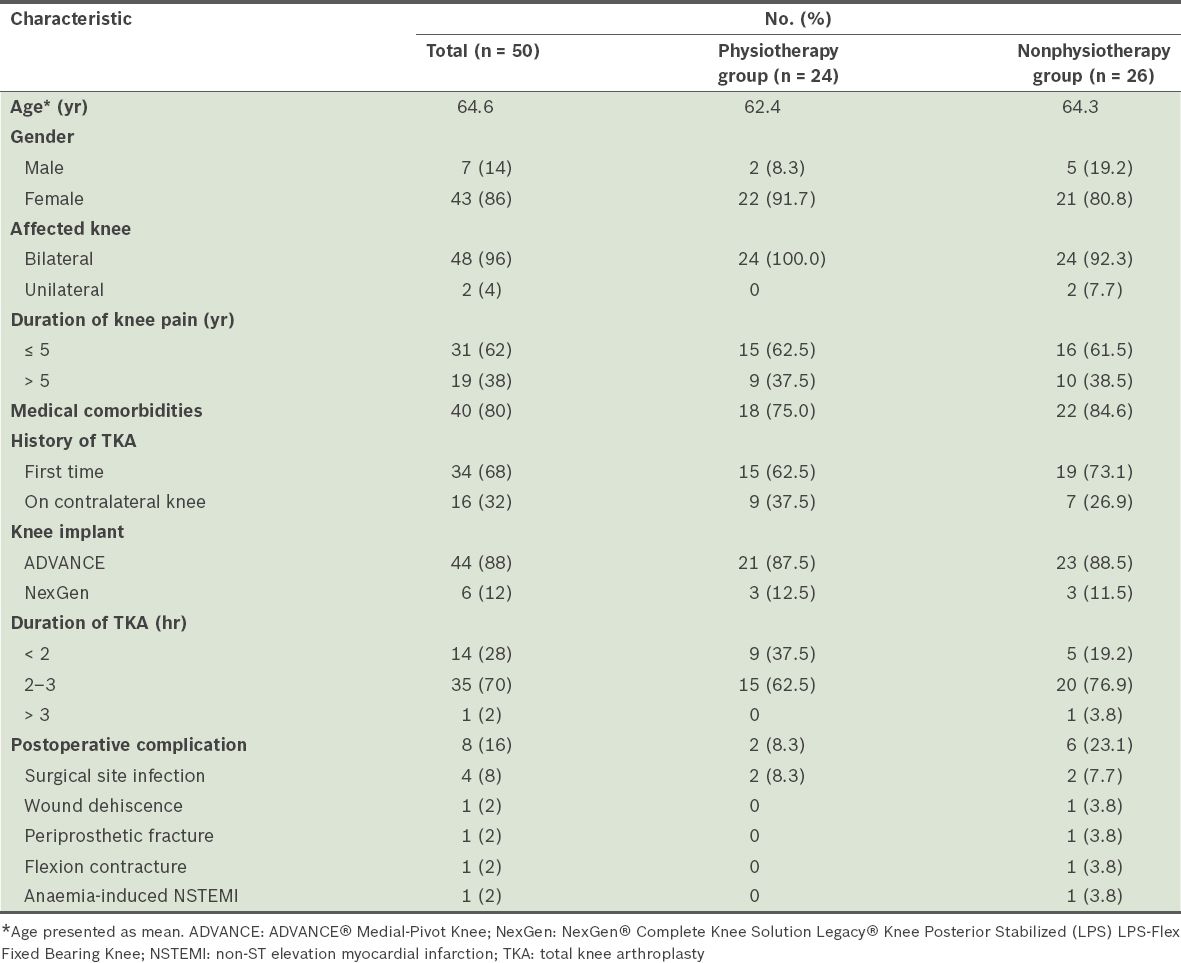
Among the 50 patients recruited for the study, 86% (n = 43) were female. The mean age of the study population was 64.6 (range 47.0–79.0) years and the age group distribution was equal in both treatment groups. One patient in the physiotherapy group had primary knee osteoarthritis and underwent surgery at the age of 47 years for severe pain. All patients who were recruited returned for follow-up. Patients in the physiotherapy group fully complied with the physiotherapy programme. The sociodemographic and medical data of the participants is summarised in
Table III
Sociodemographic and medical data of the study population.
Repeated measures ANOVA performed within groups showed that there was a significant difference in mean score within all KOOS subscales when scores at different times were compared (p < 0.001). However, apart from the ROM score, there was no significant difference between postoperative scores at six weeks and those at three months in the nonphysiotherapy group (
Table IV
Comparison of Knee Injury and Osteoarthritis Outcome Score subscales and knee range of motion (ROM) within treatment groups over time (n = 50).
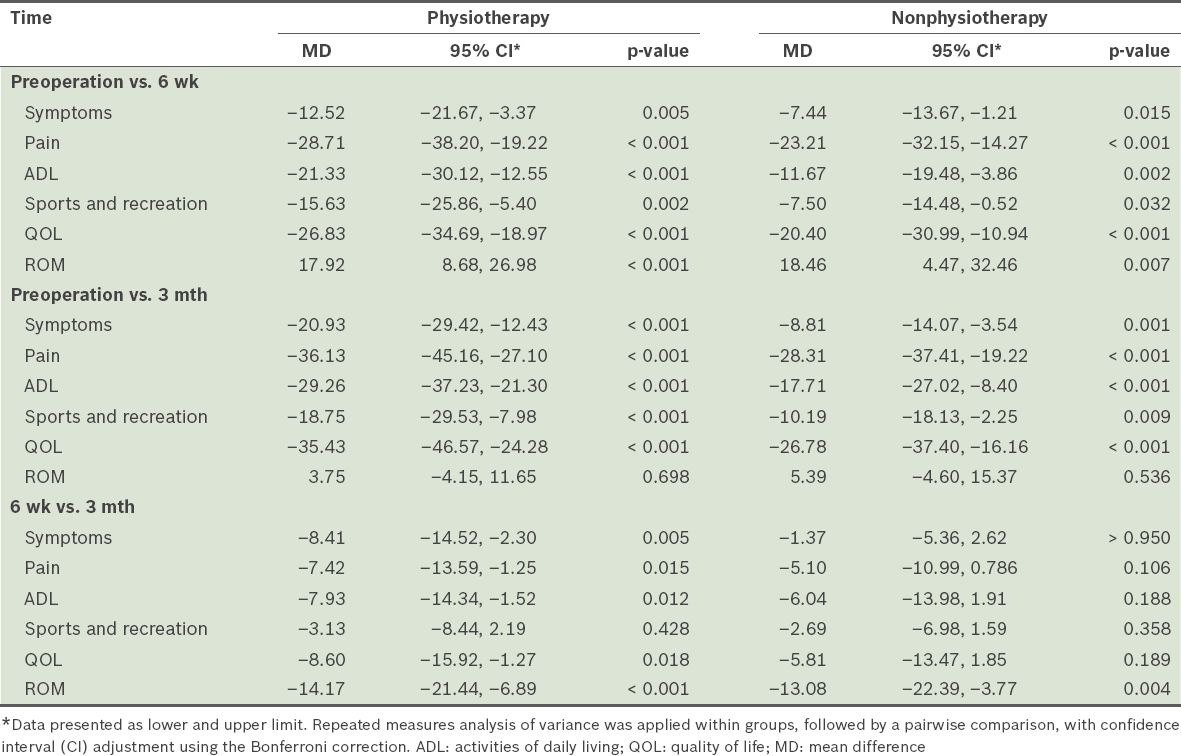
In the symptoms subscale, the mean score of the physiotherapy group did not overlap with the confidence interval (CI) of the nonphysiotherapy group at three months postoperatively, indicating that there was a significant difference in mean scores between the groups at that point. Similarly, the mean score of the physiotherapy group did not overlap with the CI of the nonphysiotherapy group at six weeks and three months in the ADL function subscale. However, in the QOL subscale, the mean score of the physiotherapy group overlapped with the CI of the nonphysiotherapy group preoperatively, and postoperatively at six weeks and three months, indicating no significant difference. Even though the mean scores of each group in the sports and recreational subscales did not overlap with the CIs of the other group (
Table V
Comparison of mean Knee Injury and Osteoarthritis Outcome Score subscales and knee range of motion (ROM) between the treatment groups over time (n = 50).
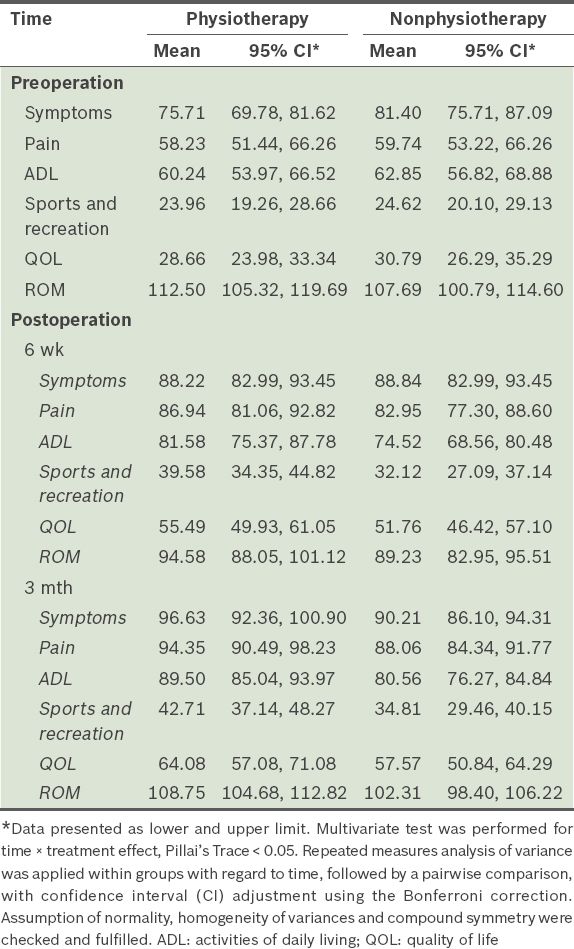
Repeated measures ANOVA performed within groups showed that mean ROM scores were significantly different when scores at different times were compared (p < 0.001); when performed between the groups, mean ROM scores were not significantly different (p = 0.928). Furthermore, there was no significant difference between preoperation and three-month ROM in both groups (
DISCUSSION
The majority of the patients were female. This was consistent with the criterion of osteoarthritis, which has a strong association with the female gender and advanced age.(11) More than half of the patients experienced knee pain for less than five years; however, the duration of symptoms does not always correlate with the severity of osteoarthritis. A total of 40 patients had associated comorbid illness at the time of surgery, correlating with previous evidence showing that comorbidities could increase the risk of infection.(12) Preoperative physiotherapy did not shorten the surgical time of TKA. The majority of patients from both groups underwent surgery within 2–3 hours (62.5% in the physiotherapy group, and 76.9% in the nonphysiotherapy group). The postoperative complication rate was higher in the nonphysiotherapy group (23.1%) compared to the physiotherapy group (8.3%), and two patients from each group had superficial surgical site infection (SSI). At the time of surgery, 40 patients had associated comorbid illnesses; this correlates with previous evidence that comorbidities could increase the risk of infection.(12) In this study, all of the patients who developed SSI and postoperative wound dehiscence had underlying diabetes mellitus at the time of surgery. Otherwise, the incidence of postoperative complications in this study was comparable with that of other studies.(13,14)
Overall analysis of the five subscales of the KOOS showed that significant improvement was seen after TKA in both groups. Patients who underwent TKA had significant improvement in symptom and functional outcomes, regardless of whether they underwent preoperative physiotherapy or not. The statistical results for KOOS subscales correlated with previous reports suggesting that TKA improved functional status, relieved pain and resulted in relatively low perioperative morbidity.(13) Findings for the sports and recreational subscale were consistent with the results of another report on local osteoarthritis populations.(15)
Statistical results for ROM showed that preoperative physiotherapy did not have a significant impact on postoperative knee ROM, as both groups showed no significant differences between ROM measurements preoperatively and at three months (
Our study had a few limitations, including its small sample size due to logistical reasons and interventions that might not be suitable for elderly patients accustomed to a sedentary lifestyle.
Previous studies reported similar insignificant results. In a randomised trial involving 39 patients by Weidenhelm et al, the preoperative physiotherapy regime used did not demonstrate any major benefits in patients (n = 19),(5) while D’Lima et al suggested that a short duration of physical therapy is not sufficient for patients with chronic arthritis.(6) A trial involving 108 patients (including 45 patients for TKA) revealed that both the physical therapy and control groups for TKA showed a similar response.(7) A systematic review of five randomised controlled trials concluded that preoperative physiotherapy programmes were not effective in improving outcomes after TKA, although their effect on total hip replacement cannot be adequately determined.(8)
In conclusion, preoperative physical therapy did not have a significant impact on the postoperative functional outcome of primary TKA in KOOS and ROM assessments. Patients experienced significant improvement in symptoms, pain, ADL and QOL subscales and ROM, although there was no significant improvement in the sports and recreational subscale after TKA, regardless of patients’ involvement in preoperative physiotherapy. Hence, we do not recommend a more intensive course of physiotherapy regime prior to TKA surgery.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Azriani Abdul Rahman from the Department of Community Medicine, Universiti Sains Malaysia, for the statistical analysis, and Mrs Anis Kausar Ghazali from the Physiotherapy Unit of HUSM. Our deepest gratitude goes to Mrs Nazmi Liana Azmi from the Clinical Research Centre, Hospital Raja Perempuan Zainab II, for her contribution to the publication of this study. An abstract of this study was presented as a poster presentation and received the Best Poster Presentation Award at Kelantan Research Day, 2013, organised by the State Clinical Research Centre.


