Abstract
A 68-year-old woman presented with weight loss of 7 kg over two years. Clinical examination revealed no specific abnormality and the patient was otherwise asymptomatic. Chest radiography performed to screen for malignancy revealed a soft tissue opacity projected over the mediastinum. Computed tomography of the thorax showed an enhancing anterior mediastinal mass with heterogeneous enhancement and contrast pooling in the arterial phase, followed by homogeneous enhancement in the venous phase, consistent with an aneurysm arising from the superior vena cava. This case highlights superior vena cava aneurysms as extremely rare causes of anterior mediastinal masses. Other causes of anterior mediastinal masses were also discussed.
CASE PRESENTATION
A 68-year-old woman presented with weight loss of 7 kg over two years. Colonoscopy and gastroscopy findings were normal. Clinical examination revealed no specific abnormality and the patient was otherwise asymptomatic.
Chest radiography (
Fig. 1
Posteroanterior chest radiograph.
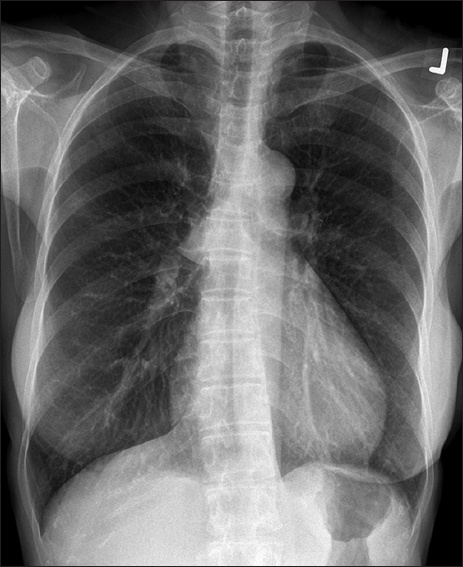
Fig. 2
(a) Arterial and (b) venous phase CT images of the chest. (c) Sagittal maximum intensity projection image of a CT aortogram.
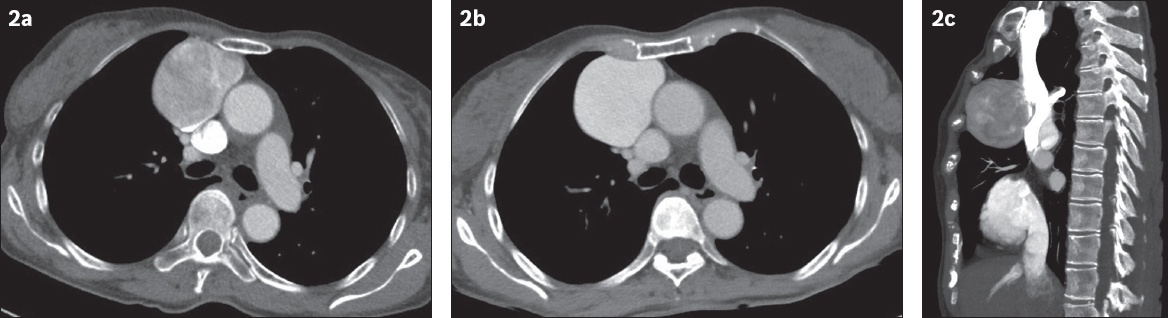
IMAGE INTERPRETATION
The chest radiograph (
DIAGNOSIS
SVC aneurysm.
CLINICAL COURSE
The patient was asymptomatic and had no complications such as thrombosis, rupture or pulmonary embolism. As she was not keen on intervention, a decision was made for conservative management and follow-up CT of the chest to monitor for interval increase in the size of the mass and complications. Follow-up CT done seven months later showed the mass to be stable in size and appearance, with no complications.
DISCUSSION
SVC aneurysms are extremely rare, with only 43 cases reported to date.(1) They are usually asymptomatic and discovered incidentally, as in our case. It has been postulated that congenital weakness in the SVC wall or absence of the longitudinal muscle layer in the tunica adventitia may predispose a patient to development of this entity. Post-trauma or postoperative causes (e.g. after a Glenn shunt or Fontan procedure) have also been reported. SVC aneurysms may be fusiform or saccular in shape, with saccular aneurysms being less common. Only 15 cases of saccular aneurysms have been reported to date.(1)
These lesions can be complicated by rupture,(2) compression of surrounding structures, thrombus formation and subsequent pulmonary embolism,(3) especially in saccular aneurysms. There are no established guidelines on the management of SVC aneurysms. It has been suggested that asymptomatic aneurysms with diameters < 40 mm can be managed conservatively with periodic scans and anticoagulation.(4) This is especially so for fusiform aneurysms that have lower complication rates.(5) Thrombolytic therapy with recombinant tissue plasminogen activator was deemed to be harmful in one case, in which mobilisation of the thrombus in the SVC aneurysm resulted in recurrent pulmonary embolism.(3) Surgical resection, usually through a median sternotomy approach, has been advocated for saccular aneurysms due to risks of complications,(1) and for aneurysms that are larger than 40 mm, growing or symptomatic, or those that contain thrombi.(4) Cardiopulmonary bypass should be used when operating on saccular or complex aneurysms, such as those with venous obstruction, calcification or thrombus formation, to prevent pulmonary embolism.(4,6) Endovascular approaches can be considered for patients with high surgical risk. In one case report, a stent was deployed into the SVC and stent meshes were then used for coil occlusion of the neck of the aneurysm sac.(7) Another case was described in which balloon-protected transcatheter thrombin injection was used in the management of a large saccular SVC aneurysm.(8)
SVC aneurysms are difficult to differentiate from other mediastinal masses such as the classical four T’s of anterior mediastinal masses, namely thymoma, teratoma, thyroid nodule and terrible lymphoma. Contrast-enhanced CT can be used to differentiate the various lesions. On chest radiographs, SVC aneurysms usually appear as anterior mediastinal masses that are commonly projected over the right hilum but have the hilum overlay sign, suggesting an anterior relation to the hilum. The hilum overlay sign refers to the hilum being visible through the mass on radiographs; this implies that the mass is not at the hilum itself, as it would obliterate the silhouette of the hilum. On CT, the enhancement pattern of the SVC aneurysm is similar to that of the SVC, and contrast layering is seen in the dependent portion of the aneurysm in the arterial phase before filling the whole aneurysm in the venous phase, likely due to slow flow. Bubbles within the mass, due to gas inadvertently introduced into the bloodstream during injection of the contrast medium, are also a clue to the diagnosis of a vascular lesion.(1) The communicating channel with the SVC is not always seen but can appear as a stalk-like channel.(9)
In contrast, a mediastinal tumour such as a thymoma typically manifests as a homogeneously enhancing anterior mediastinal mass with smooth or lobulated contours, located anywhere from the thoracic inlet to the cardiophrenic angle. Heterogeneity due to calcification, necrosis, cystic change (
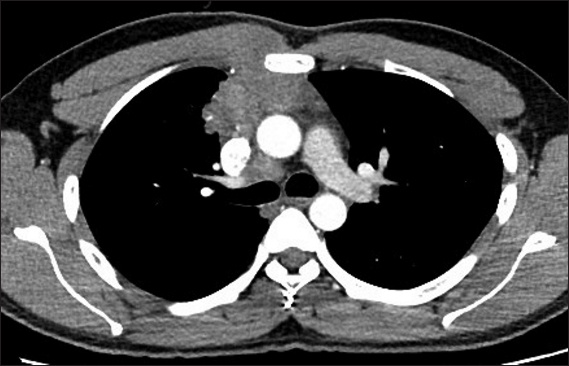
Fig. 3
A mediastinal mass found in a 73-year-old woman on routine chest radiography. Axial contrast-enhanced CT image shows a well-defined mass at the anterior mediastinum with generally homogeneous soft tissue density and a central cystic focus. The enhancement along the lateral surface of the mass is a vessel. Thymectomy was performed and a diagnosis of thymoma was made histologically.

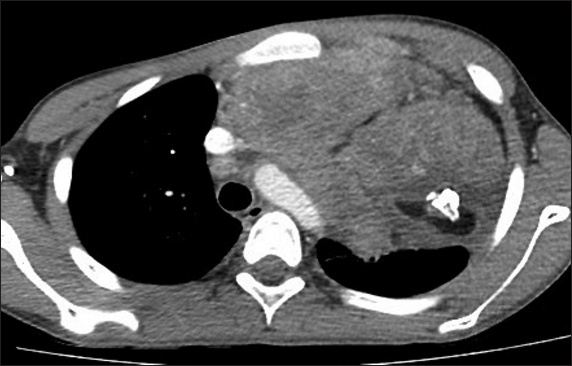
Primary mediastinal lymphoma (
Fig. 4
A palpable mass at the right parasternal region in a 31-year-old man. Axial contrast-enhanced CT image shows an irregularly outlined soft tissue density mass, which is seen invading into the anterior chest wall on the right and involving the pectoralis major muscle. The mass is largely homogeneous in enhancement and conforms to the shape of the vessels. Chamberlain procedure was performed and tissue biopsy showed composite lymphoma consisting of nodular sclerosing Hodgkin lymphoma and peripheral T-cell lymphoma.
On CT, teratomas are distinct in appearance, with fluid, soft tissue, calcification and fat content (
Fig. 5
Axial contrast-enhanced CT image shows a large mediastinal mass compressing the left lung of a 16-year-old boy who presented with cough of one month’s duration and breathlessness, probably causing his symptoms. Fat content and a tooth are seen within the predominantly solid mass, consistent with a mature teratoma. The diagnosis was confirmed histologically.
A retrosternal thyroid goitre extension may be mistaken for a mediastinal mass on chest radiography, but should be fairly obvious on CT, as it is contiguous with the thyroid gland (
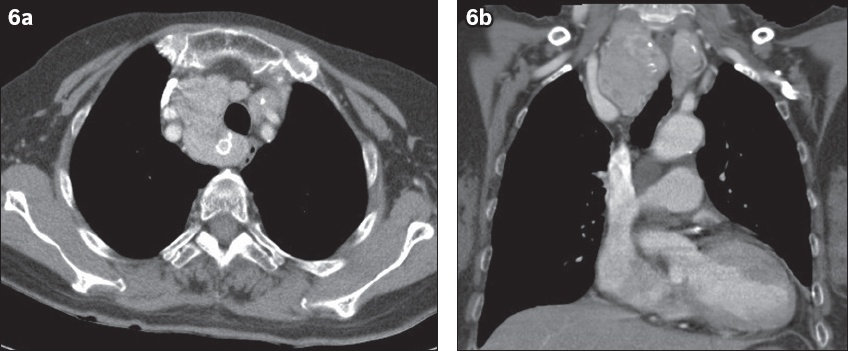
Fig. 6
A neck mass that was gradually increasing in size in a 71-year-old woman. (a) Axial and (b) coronal contrast-enhanced CT images show nodular heterogenous thyroid goitre with retrosternal extension into the upper mediastinum. Fine needle aspiration cytology favoured nodular goitre with cystic changes.
In conclusion, SVC aneurysm is a rare cause of an anterior mediastinal mass that can be mistaken for one of the more common mediastinal masses. However, careful evaluation with contrast-enhanced CT can usually reveal the vascular nature of the lesion. CT angiography, with a combination of arterial and venous phases, can help to further confirm this. This is essential to avoid biopsy of the lesion, which would be catastrophic, and is also useful for planning of management.
SMJ-60-21.pdf
ACKNOWLEDGEMENT
The authors would like to thank Dr Sandeep Halagatti Venkatesh for his contribution to the case.


