CASE PRESENTATION
A 69-year-old woman with a history of cervical carcinoma underwent a total hysterectomy, bilateral salpingo-oophorectomy and pelvic lymph node dissection followed by chemoradiotherapy. She developed radiotherapy-related ureteral strictures requiring long-term ureteric stents.
Three years after the implantation of the ureteric stents, she presented with recurrent gross haematuria. Extensive investigations with serial computed tomography (CT) studies, flexible cystoscopy, ureteroscopy and retrograde pyelogram failed to reveal a cause and she was diagnosed with radiation cystitis. Her existing ureteric stents, which were thought to be exacerbating factors, were removed and bilateral nephrostomies were placed.
She subsequently suffered an episode of massive haematuria and hypotension with blood pressure of 70/50 mmHg. Laboratory tests revealed a drop in haemoglobin level from 10 g/dL to 6 g/dL. CT angiography of the abdomen and pelvis (
Fig. 1
Contrast-enhanced CT angiogram of the lower abdomen in (a) axial, (b) coronal and (c) magnified consecutive axial view.
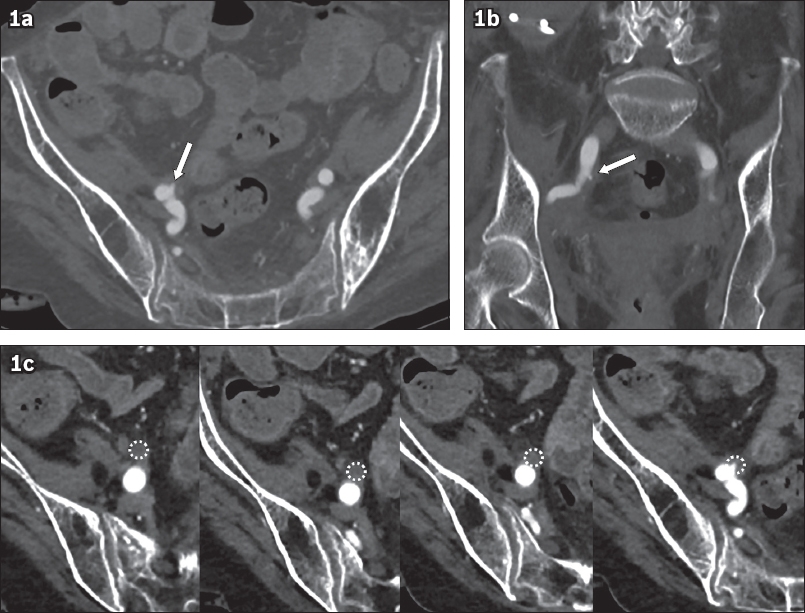
Fig. 2
Digital subtraction angiograms of the right common iliac artery.
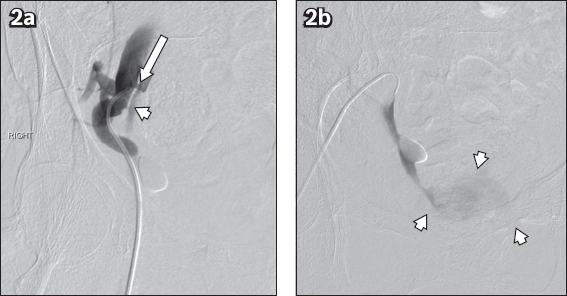
IMAGE INTERPRETATION
Arterial phase axial and coronal CT images show a tiny outpouching arising from the right common iliac artery (arrow,
Digital subtraction angiography (DSA;
DIAGNOSIS
Arterioureteral fistula (AUF).
CLINICAL COURSE
The diagnosis of AUF was ultimately only made during catheter angiography, which was performed with a view to carrying out arterial embolisation. Initial selective angiography of both renal arteries and the left internal iliac artery did not reveal a source of haemorrhage.
The right common iliac artery was accessed with a 5-Fr Cobra C2 catheter. A non-selective angiographic run performed in an attempt to cannulate the right internal iliac artery resulted in opacification of the right ureter, diagnostic of an AUF (
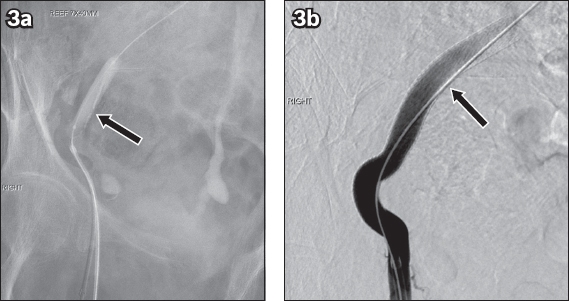
Fig. 3
(a) Angiogram shows balloon tamponade of the haemorrhage into the right ureter using a 7 mm × 40 mm balloon catheter (arrow) and (b) an 8 mm × 100 mm Gore® Viabahn® stent-graft (arrow) placed across the arterioureteral fistula, occluding it with no further contrast flow into the right ureter.
The patient remained well post intervention with no further episodes of haematuria to date.
DISCUSSION
AUF is a rare cause of haematuria resulting from fistulous communication between the ureter and the aorta or iliac artery. Primary AUFs (15%) arise from arterial pathologies such as aortoiliac aneurysms or arteriovenous malformations that erode into the ureter.(1,2) Secondary AUFs (85%) are more common and result from malignancy, surgery, radiotherapy or ureteric stents, which trigger chronic inflammation and fibrosis, leading to adhesion and eventual fistulation of the fragile ureter and adjacent pulsatile artery.(3,4) This was the likely process in our patient, who had a history of gynaecological malignancy treated with surgery, radiotherapy and ureteric stents, all of which are well-known risk factors for developing secondary AUF. While AUF is an uncommon condition, its incidence is increasing as ageing populations undergo aggressive cancer treatment. To date, at least 139 cases have been reported in the literature.(2,5)
Patients with AUF present with haematuria, which may or may not be associated with flank pain.(2) The degree of haematuria can range from intermittent haematuria to life-threatening massive haematuria with a mortality rate of 13%.(2,5) Due to its non-specific presentation, more common causes of gross haematuria such as radiation cystitis (
Fig. 4
An 80-year-old woman with a history of cervical cancer treated with radiotherapy presented 20 years later with gross haematuria. Axial contrast-enhanced CT image shows circumferential thickening and irregularity of the bladder wall with surrounding fat stranding compatible with radiation cystitis.
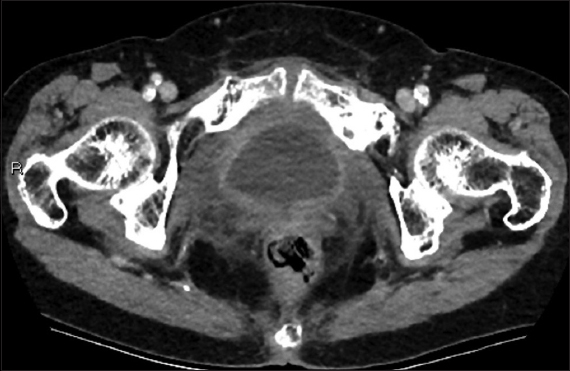
Fig. 5
A 50-year-old man presented with gross haematuria. Axial contrast-enhanced CT image shows an enhancing soft tissue lesion (arrows) at the right vesicoureteric junction. Cystoscopy confirmed a solid mass at this location and histology revealed papillary urothelial carcinoma.
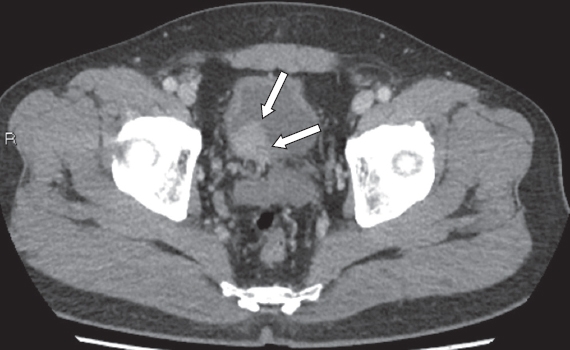
Cystoscopic evaluation may reveal pulsatile bleeding from the ureteral orifice alluding to an AUF, but this may be absent at the time of examination.(2) CT is reported to be only moderately useful and often yields non-specific findings such as hydronephrosis and blood clots within the urinary system, also demonstrated in this case (
Fig. 6
A 69-year-old woman who developed radiotherapy-related ureteral strictures requiring long-term ureteric stents underwent CT imaging for recurrent haematuria while the ureteric stents were in situ. Axial contrast-enhanced CT image shows non-specific findings of bilateral hydronephrosis (arrowheads) with hyperdense blood products (arrow) within the right pelvicalyceal system.
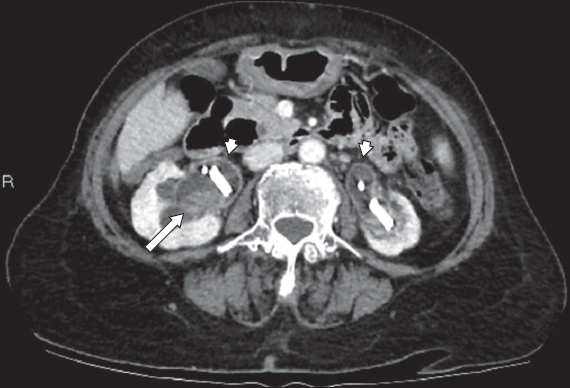
AUFs occur at the region of the ureteric crossing; in the native ureter, this is usually at the distal common iliac artery with less common sites being the external or internal iliac arteries.(2) In patients with urinary diversion, the proximal common iliac artery or distal abdominal aorta may be involved instead.(2) Massive haematuria in a patient with risk factors should prompt a targeted review of these areas using CT for the presence of a pseudoaneurysm.
Direct fistulous communication between the artery and ureter is difficult to demonstrate without DSA, which remains the gold standard in the imaging diagnosis of AUF with a reported sensitivity of 69%.(2,5) Findings on DSA may range from subtle arterial wall irregularity or pseudoaneurysm to active extravasation of contrast into the ureter.(2) To optimise the diagnostic yield of CT and DSA, ureteric stents should be removed to allow visualisation of contrast flow into the ureter. Unfortunately, false negative angiography studies are possible and provocative manoeuvres may be required. One previously described technique is the use of a balloon catheter to sweep across the ureter at the suspected point of fistulation while an arteriogram is obtained from an ipsilateral arterial access to demonstrate contrast extravasation into the ureter.(9)
Previously, AUFs were treated by surgical repair of the involved artery and ureter, which is particularly difficult in patients who have adhesions from surgery and radiotherapy. Currently, the most commonly performed procedure is endovascular treatment with balloon tamponade of the haemorrhage before placement of a stent graft across the fistula, while other techniques such as coil embolisation of the affected artery are less common.(2)
The literature on the long-term outcome of endovascular treatment in patients with AUF is currently sparse. A small study of 14 cases reported complications such as lower limb ischaemia, deep vein thrombosis, skin ulceration, chronic leg pain, femoral head osteonecrosis, limb amputation and recurrent haemorrhage.(10)
In conclusion, AUF is a relatively rare cause of haematuria, but its incidence is increasing as more pelvic cancers are detected and treated aggressively. CT findings may be non-specific, and a high index of suspicion is required when interpreting studies of patients with risk factors. DSA remains the gold standard for imaging diagnosis and allows for concomitant endovascular management, which is now favoured over surgical repair.
SMJ-61-330.pdf


