Abstract
INTRODUCTION
In our national emergency dispatch centre, the standard protocol for dispatcher-assisted cardiopulmonary resuscitation (DACPR) in out-of-hospital cardiac arrests (OHCAs) involves the instruction ‘push 100 times a minute 5 cm deep’. As part of quality improvement, the instruction was simplified to ‘push hard and fast’.
METHODS
We analysed all dispatcher-diagnosed OHCAs over four months in 2018: January to February (‘push 100 times a minute 5 cm deep’) and August to September (‘push hard and fast’). We also performed secondary per-protocol analysis based on the protocol used: (a) standard (n = 48); (b) simplified (n = 227); and (c) own words (n = 231).
RESULTS
A total of 506 cases were included: 282 in the ‘before’ group and 224 in the ‘after’ group. Adherence to the protocol was 15.2% in the ‘before’ phase and 72.8% in the ‘after’ phase (p < 0.001). The mean time between instruction and first compression for the ‘before’ and ‘after’ groups was 34.36 seconds and 26.83 seconds, respectively (p < 0.001). Time to first compression was 238.62 seconds and 218.83 seconds in the ‘before’ and ‘after’ groups, respectively (p = 0.016). In the per-protocol analysis, the interval between instruction and compression was 37.19 seconds, 28.31 seconds and 32.40 seconds in the standard protocol, simplified protocol and ‘own words’ groups, respectively (p = 0.005). The need for paraphrasing was 60.4% in the standard protocol group and 81.5% in the simplified group (p < 0.001).
CONCLUSION
Simplified instructions were associated with a shorter interval between instruction and first compression. Efforts should be directed at simplifying DACPR instructions.
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) remains a serious global concern.(1,2) Over 2,400 OHCAs occur in Singapore every year.(3) Previous studies have shown that dispatcher-assisted cardiopulmonary resuscitation (DACPR) is essential in reducing the time to first compression and improving overall survival.(4-6)
As DACPR requires clear communication between the dispatcher and the layperson who may not know how to perform cardiopulmonary resuscitation (CPR), the actual terms used in communicating the method of CPR are important. Poor communication could lead to delay in commencement of CPR, incorrectly performed CPR, or CPR not being performed altogether and, consequently, poor patient outcomes.(7)
Untrained laypersons often do not know the rate and depth to which to compress the patient’s chest wall.(8) Out of fear of hurting the patient, they often compress it at too slow a rate and at a shallow depth, leading to ineffective CPR.(8) The American Heart Association recommends that the dispatcher instruct laypersons with the phrase ‘push 100 times a minute 5 cm deep’.(9,10) While this phrase captures the important tenets of CPR, in a life-threatening situation such as an OHCA, it may be counterproductive to attempt to teach in such great detail.(11) The optimal word choice to achieve CPR performance is not well-established.(12)
A simulation study showed that when simplified instructions were used, the mean chest compression depth was greater and met the CPR targets of the American Heart Association more often.(13) In a simulation study on DACPR, there was no difference in compression depth, quality of CPR or physical strain on lay rescuers with the use of simplified instructions.(14) Another simulation study showed that a simplified DACPR script was superior to the conventional script in terms of time to first compression.(5,15) It is unclear whether these simulation studies would translate to real-world gains. Our prospective, before-and-after, opportunistic real-world study sought to investigate whether simplified instructional phrasing would improve the time interval between instruction and first compression.
METHODS
The single national dispatch centre in Singapore serves a population of 5.6 million.(16) The dispatch centre processed 182,502 emergency medical calls in 2017, which translated to about 500 calls daily.(3) As Singapore is a multiracial, multilingual society, an estimated 15% of calls are not purely in English. English, as spoken in Singapore, is commonly a variant called Singlish, which includes local phrases that are co-opted from Malay, Mandarin and a variety of Chinese dialects. If the caller is unable to communicate functionally in English, a dispatcher familiar with the caller’s preferred language is requested to take over the call. If DACPR is required, the dispatcher translates the DACPR instructions from English to the language being used when giving the instructions, but owing to the nature of the languages (e.g. Chinese dialects or Malay), a lot of paraphrasing is involved. There is currently no standardised script for a dispatcher to use if the instructions for DACPR are not in English.
As part of a quality improvement project, our dispatch centre changed the recommended phrasing from ‘push 100 times a minute 5 cm deep’ to ‘push hard and fast’. Dispatchers were allowed to use alternative phrasing based on the exigencies of the call. In this study, we examined all OHCA calls to evaluate the effectiveness of the new phrasing. Training for the new phrasing started in March 2018 and was completed by May 2018. The dispatchers were given two more months until end July 2018 for familiarisation.
Two trained data abstractors reviewed all telephone records of OHCAs over a four-month period in 2018 by listening to the audio recordings that were retrieved from the system. Calls from January to February 2018 were placed in the ‘before’ group, and those from August to September 2018 were in the ‘after’ group. The first instruction given was used to indicate the group the call was assigned to. For example, if the dispatcher used the phrase ‘push hard and fast’ first, the call would be assigned to the ‘after’ group.
The instruction for DACPR was considered to be given when the dispatcher instructed the caller to put a hand on the centre of the chest, with the timer starting when the caller said the word ‘chest’. The time of first compression was defined as the point where the caller or dispatcher first counted out the chest compression audibly and the word ‘one’ was heard.
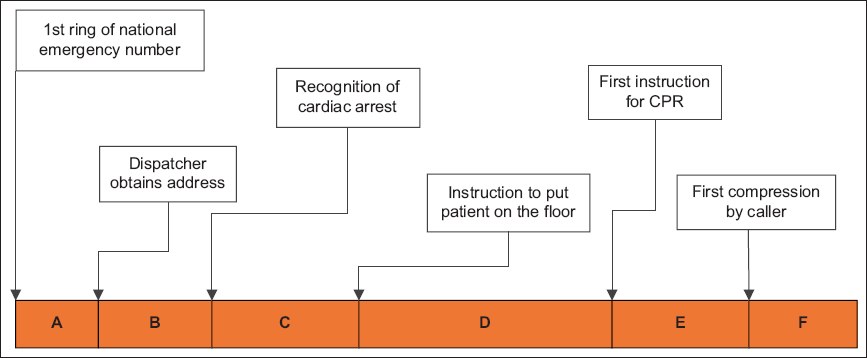
Primary analysis was performed based on intention to treat. We defined compliance as using the phrasing ‘push 100 times a minute 5 cm deep’ in the ‘before’ phase and ‘push hard and fast’ in the ‘after’ phase. Secondary analysis was performed on a per-protocol basis. Cases were assigned to three groups: (a) ‘push 100 times a minute 5 cm deep’, (b) ‘push hard and fast’ and (c) own words, in which the dispatchers used neither of the suggested protocol phrasings to give instructions for DACPR. The need for paraphrasing was defined as the presence of any alternative phrasing used during the call other than repeats of the initial phrasing when reviewing the audio records. When a call taker used a term other than ‘push 100 times a minute 5 cm deep’ or ‘push hard and fast’, he was deemed to have used his own words. Outcomes were determined a priori. The primary outcome was the time interval between instruction and compression (time segment E in
Fig. 1
Timeline shows the stages of dispatcher-assisted cardiopulmonary resuscitation (CPR). A + B = time to recognise cardiac arrest; A + B + C + D = time to instructions for CPR; A + B + C + D + E = time to first chest compression; E: interval between instruction and first compression
The study was exempted from Centralised Institutional Review Board approval (reference 2018/2937), as it used de-identified data from national cardiac arrest audit and quality improvement registry under the Ministry of Health’s Unit for Prehospital Emergency Care.
As this was an opportunistic real-world study, all cases in the study period were included. The following cases were excluded: (a) OHCAs for which compressions were not given; (b) OHCAs for which instruction for CPR or counting of first compressions was not audible; and (c) non-English calls.
All statistical analysis was performed using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA). For quantitative outcomes, we calculated the mean and its corresponding 95% confidence intervals. For qualitative outcomes, we calculated the odds ratio and its 95% confidence interval. Continuous variables were evaluated using one-way analysis of variance with Bonferroni correction, while categorical variables were evaluated using Pearson’s chi-square test. A p-value < 0.05 was considered statistically significant.
RESULTS
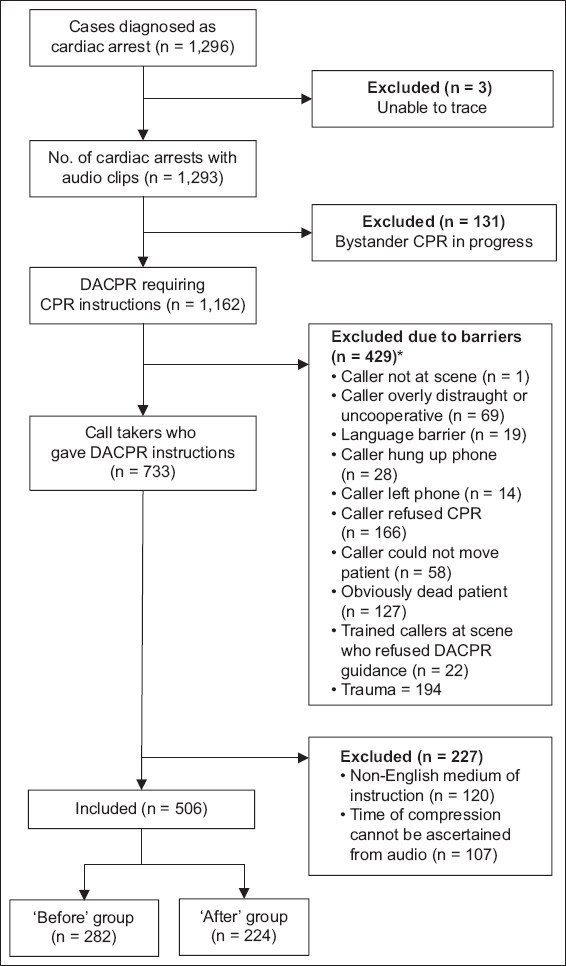
A total of 1,296 cases were retrieved for the study. 16.4% of all cases in which DACPR instructions were given were excluded because the instructions were not given in English. After the exclusions were applied, a total of 506 cases were selected and divided into two groups, 282 (55.7%) in the ‘before’ group and 224 (44.3%) in the ‘after’ group (
Fig. 2
Flowchart shows study enrolment and key exclusions. *121 cases had > 1 barrier. CPR: cardiopulmonary resuscitation; DACPR: dispatcher-assisted CPR
The characteristics of patients and calls are listed in
Table I
Characteristics of patients and calls.
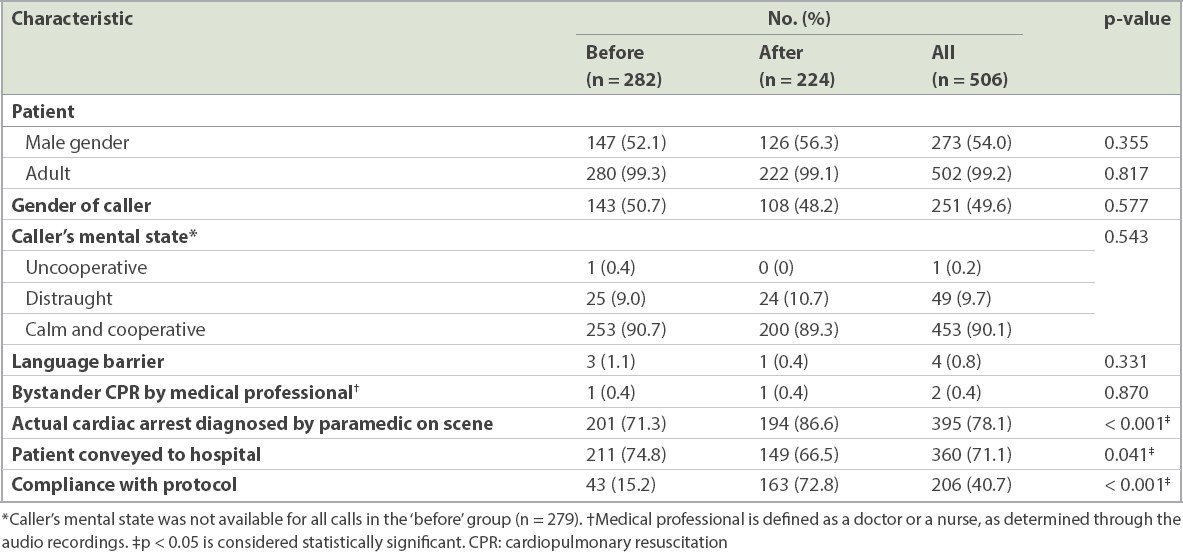
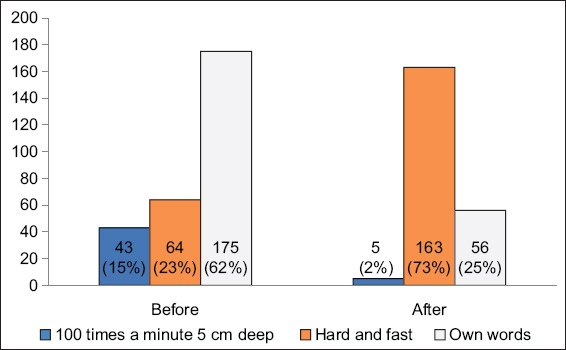
Fig. 3
Graph shows a breakdown of phrasing used in the ‘before’ and ‘after’ groups.
The main results with primary and secondary outcomes are detailed in Tables
Table II
Primary and secondary outcomes in the intention-to-treat analysis.
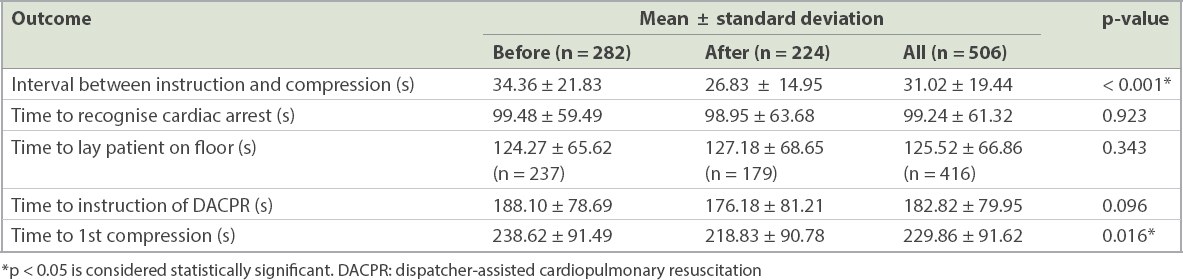
Table III
Primary and secondary outcomes in per-protocol analysis.
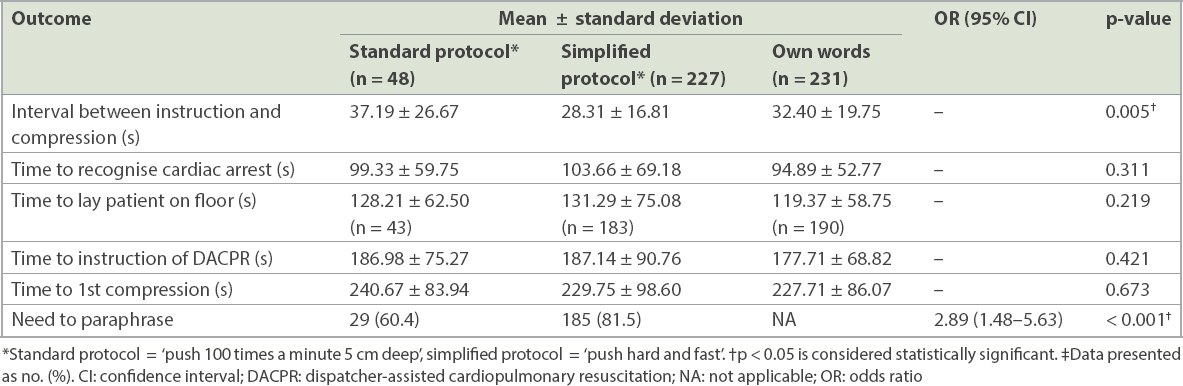
In the per-protocol analysis, there were 48 (9.5%) in the standard protocol ‘push 100 times a minute 5 cm deep’ group, 227 (44.9%) in the simplified protocol ‘push hard and fast’ group and 231 (45.7%) in the ‘own words’ group. The simplified protocol was shown to have the shortest interval between instruction and compression, with a significantly higher need to paraphrase.
DISCUSSION
Our study found that compliance to protocol and use of the phrase ‘push hard and fast’ was associated with a faster time to first compression and shorter interval between instruction and compression. In addition, the phrase was associated with more paraphrasing compared to the conventional phrasing.
Compliance to protocol remained a major limitation. The intervening months during which training was conducted for dispatchers to use the new phrasing could have led to increased emphasis on DACPR, consequently affecting the time to first compression. While strict protocol compliance has not been shown to have an effect on dispatcher OHCA identification, correct application of the protocol was likely to be a major factor that led to better primary outcomes.(17) It is possible that the simplification of instructions in itself facilitated adherence to the protocol. Protocol compliance remains an important cornerstone of good-quality DACPR and should be reinforced periodically.
Notwithstanding the limitation of poor compliance, our per-protocol analysis continued to show improved outcomes with simplified instructions. Good-quality DACPR is heavily dependent on the verbal communication process. Several studies have shown that the linguistic choices of dispatchers, particularly their assertiveness, affected callers’ agreement to perform CPR and other DACPR metrics.(6,18-20) Our study demonstrated that a high-information message was associated with a longer time to first compression. In a high-stress situation for the lay caller, more information could paradoxically lead to information overload. This occurs when ‘the amount of input to a system exceeds its processing capacity’.(21,22) When too much CPR is taught in a short time, the unintended outcome is lower-quality CPR. Our study confirms findings from prior simulation studies that longer CPR instructions are associated with poorer quality of CPR. When compared with simplified instructions, Painter et al(17) demonstrated that conventional DACPR instructions to lay callers were associated with longer time to first compression.
Simplified DACPR instructions are of particular importance in societies where English proficiency is limited. While English is the most commonly used language in Singapore, proficiency in the language varies among populations.(23) Meischke et al(11) have shown that language proficiency has a significant impact on the quality of DACPR. Limited language proficiency was shown to increase the need for paraphrasing.(24) Examples of paraphrasing used included ‘press 5 cm deep and follow my count’ or ‘use your body weight to compress 5 cm deep upon my count’. It is surprising that simplified instructions required more paraphrasing. This could be because simplified instructions did not provide sufficient information or because dispatchers felt the need to further elaborate on simple instructions. It is unclear whether paraphrasing helped improve the caller’s comprehension of instructions. Taking into account the different levels of language proficiency and comprehension of the population, we believe that some paraphrasing should be allowed. Dispatchers typically use word variations to convey similar messages. Where feasible, dispatchers should check the callers’ comprehension of the instructions given.
In telecommunication, the transmission process is influenced by other technical factors such as the volume, voice quality of the speaker mode of the caller’s phone and ambient environmental noise.(25,26) Hence, shorter phrases would have a better chance of complete transmission and reception. Likewise, shorter phrases in non-English languages should be considered, as 16.3% of DACPR instructions during the study period were given in languages other than English. Technological innovations such as the use of smartphone applications and video calls have the potential to enhance the quality of verbal instructions through the addition of a visual component.
Lastly, in such rare, time-sensitive scenarios, the ability to understand dispatchers’ instructions is limited.(26-28) It is highly stressful for the lay caller to perform CPR, a relatively complex procedure, with only telephonic guidance.(14,29,30) It is imperative that instructions are clear and succinct. Indeed, DACPR is a situation in which ‘less is more’. Findings from our study offer further opportunities to improve DACPR instructions.
Besides the limitation of poor compliance in the ‘before’ phase as mentioned above, this study had several limitations. Firstly, the before-and-after study design has its inherent limitations, is subject to allocation bias and is affected by temporal trends. Nonetheless, we believe that emphasis on dispatcher compliance and the introduction of simplified phrasing would result in real-world gains. Secondly, taking the first phrase used, we completed our analysis based on one CPR phrase per call and could not account for the effect of immediate paraphrasing. Thirdly, the intervention group had the highest proportion of true cardiac arrests, as determined by on-scene paramedics. While multivariate analysis did not reveal this to be a significant factor, the smaller sample size may predispose the results to a Type 2 error. Finally, while we measured the time to first compression, there was no way to determine the depth of compression and whether ‘pushing hard’ would be better than ‘pushing 5 cm’. Multiple simulation studies have addressed the point that ‘pushing hard’ is just as good in achieving the desired depth of 5 cm.(10,12,15,28) Nevertheless, the strength of this study is that it is the first known real-world, national study showing that simplified phrasing results in a shorter time to first compression than traditional phrasing does.
In summary, our study showed that when giving instructions for DACPR, simplified instruction was associated with a shorter interval between the time of instruction and first compression. Efforts should be made to encourage adherence to protocols.
Dr Desmond Mao is a Consultant Emergency Medicine physician from Khoo Teck Puat Hospital, Singapore, and the first Singapore Prehospital Emergency Care-trained fellow. His research interests include prehospital medicine, out-of-hospital cardiac arrest, emergency department frequent attenders, emergency medicine and alcohol misuse.
ACKNOWLEDGEMENTS
We would like to thank the Singapore Civil Defence Force for providing the audio recordings for analysis; Mr Alvin Ee, Nursing Lecturer at the Institute of Technical Education, Singapore, for his help with the design and data collection of the study; and Ms Nur Shahidah, Senior Clinical Research Coordinator at Singapore General Hospital, Singapore, for her help in providing inputs for part of the manuscript.


