Abstract
INTRODUCTION
In Singapore, as strict laws are a strong deterrent against armed violence, little is known about the epidemiology of penetrating stab wound injuries. Our study aimed to investigate the epidemiology of stab wound injuries at a major trauma centre in Singapore and determine if there was a difference in severity between self-inflicted stab wound (SI) injuries and those inflicted by others (IO).
METHODS
We retrospectively reviewed all penetrating injuries at Tan Tock Seng Hospital, and identified and categorised all stab wound injuries as SI or IO. Basic demographic information, injury severity characteristics and outcome data were compared between these two groups. A review of all mortalities was performed, including recording the causes of death.
RESULTS
Between 2005 and 2010, there were a total of 149 stab wound injuries, of which 24 (16.1%) were SI and 125 (83.9%) were IO injuries. Patients tended to be young (mean age 34.1 ± 14.2 years). The mean Injury Severity Score was significantly different between the SI and IO groups (8.8 ± 6.5 vs. 12.3 ± 8.1; p = 0.03). In both groups, the majority underwent an operative procedure (83.3% vs. 85.6%) and had an average hospital stay of four days.
CONCLUSION
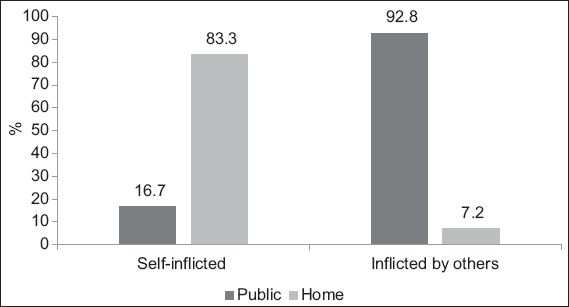
The study confirms our hypothesis that SI injuries tend to be less severe than IO injuries and are more likely to occur at home rather than at a public area. This finding may be useful in the triage of patients with stab wound injuries.
INTRODUCTION
Penetrating trauma typically involves the violation of a body cavity (e.g. thoracic or abdominal) by a gunshot or stab wound. The type of weapon has a substantial impact on the diagnostic and management process. For example, it may be generally assumed that the velocity of a penetrating bullet is higher than that of a fruit knife. This is because close-range injuries intuitively transfer more kinetic energy than those sustained from a distance. In stab wound injuries, thrusting may also transmit more force than a slash injury that inadvertently breaches the cavity.
In Singapore, strict legislation acts as a strong deterrent against armed violence.(1) Age-standardised death rates (per 100,000 population) from homicide and injury purposely inflicted by others in 1995 was reported to be low at 1.5, compared to 1.7 in Australia, 1.0 in the United Kingdom and 9.4 in the United States,(2) where weapons for self-defence are more readily available. Researchers found a total of 13,030 stab injuries at 900 American trauma centres between 2002 and 2008;(3) this is roughly equivalent to 2.4 stab wound injuries per year per trauma centre. Little is known about the epidemiology of stab wound injuries in Singapore. Additionally, we anecdotally observed that self-inflicted stab wound (SI) injuries appeared to be less severe than those inflicted by others (IO).
The aim of our study was to investigate the epidemiology of stab wound injuries at a major trauma centre in Singapore and determine if there was a difference in severity between SI and IO injuries.
METHODS
Tan Tock Seng Hospital (TTSH) is a 1,600-bed hospital in central Singapore that provides medical care to over 1.5 million people. It reportedly handles the highest number of trauma patients in Singapore, admitting over 1,000 serious trauma patients yearly (Injury Severity Score [ISS] 9 and above), hence may be considered the busiest trauma and acute care hospital in Singapore.(4)
After obtaining exempt status from our institutional review board, we reviewed the TTSH Trauma Registry, a prospectively maintained database, and identified all patients with penetrating injuries who were admitted to TTSH from 1 January 2005 to 31 December 2010. Slash injuries were not classified as penetrating. Subsequently, we identified all stab wound injuries and classified these patients into two groups, SI and IO. Basic demographic information, injury severity characteristics and outcome data were recorded and compared between these two groups. Injury severity characteristics included anatomic and physiologic measures of injury severity, namely ISS and Revised Trauma Score (RTS), respectively. Outcomes data included mortality and hospital length of stay (LOS). We also determined if the patient underwent an operation (i.e. surgical procedure requiring general anaesthesia) and excluded any patients with wound exploration under local anaesthesia undertaken at the emergency department (ED). For patients in the SI group, we recorded whether a psychiatrist reviewed the patient during the hospital stay. Finally, we examined all mortalities, identified the causes of death (as documented in the patient’s medical case records) and, if applicable, obtained the final diagnosis from a coroner’s report.
All statistical analyses were performed using SAS 9.3 (SAS Institute Inc, Cary, NC, USA). Comparisons between patient and injury characteristics were made using Fisher’s exact test for categorical variables and Mann-Whitney U test for continuous variables. A two-tailed p-value < 0.05 indicated statistical significance.
RESULTS
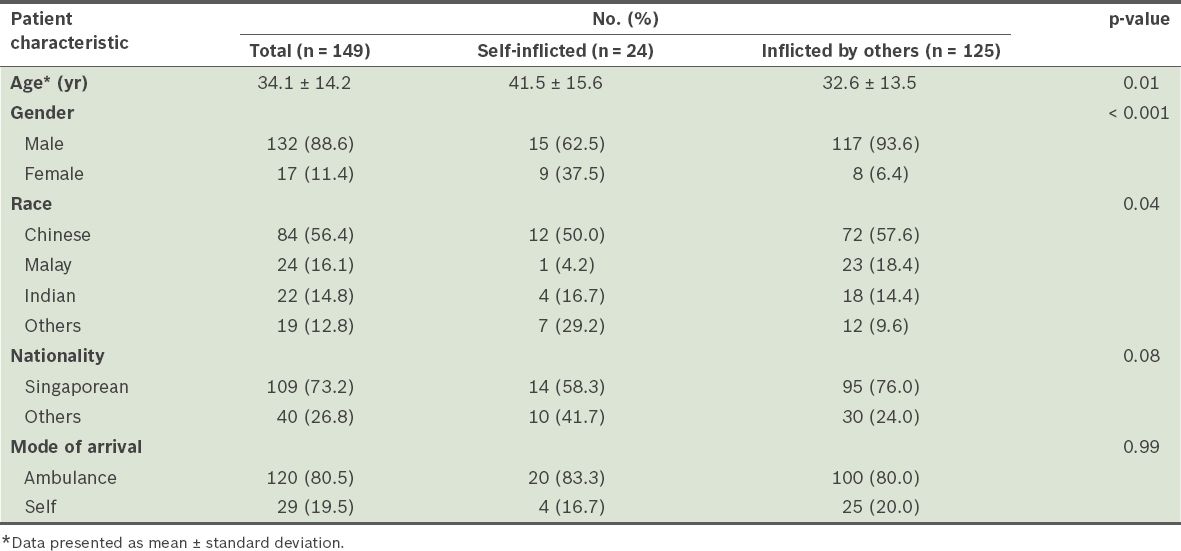
Between 1 January 2005 and 31 December 2010, there were a total of 149 stab wound injuries. Of these, 24 (16.1%) were SI and 125 (83.9%) were IO injuries. There was no significant rise in the proportion of SI or IO injuries across the study period. Mean ages for the SI and IO groups were 41.5 ± 15.6 years and 32.6 ± 13.5 years, respectively. While there was a male predominance in both groups at 88.6%, there were significantly more men in the IO than SI group (93.6% vs. 62.5%, p < 0.001) (
Table I
Patient and injury characteristics of stab wound patients.
SI injuries were significantly more likely to occur at home, while IO injuries tended to occur in public areas (p < 0.001) (
Fig. 1
Location of stab wound injuries according to category of intent.
There was no significant difference between both groups in physiologic injury severity (as indicated by average RTS) and proportion of patients presenting with a systolic blood pressure (SBP) of less than 90 mmHg. In the IO group, 3 (2.4%) patients presented with an unreportable blood pressure and pulse. Of the 20 patients in the IO group who presented with a low blood pressure of less than 90 mmHg, 9 (45.0%) were also tachycardic (i.e. in circulatory shock). This is opposed to the SI group, in which only one patient, who stabbed herself in the neck, presented with circulatory shock (
Table II
Injury severity characteristics and outcomes of stab wound patients.
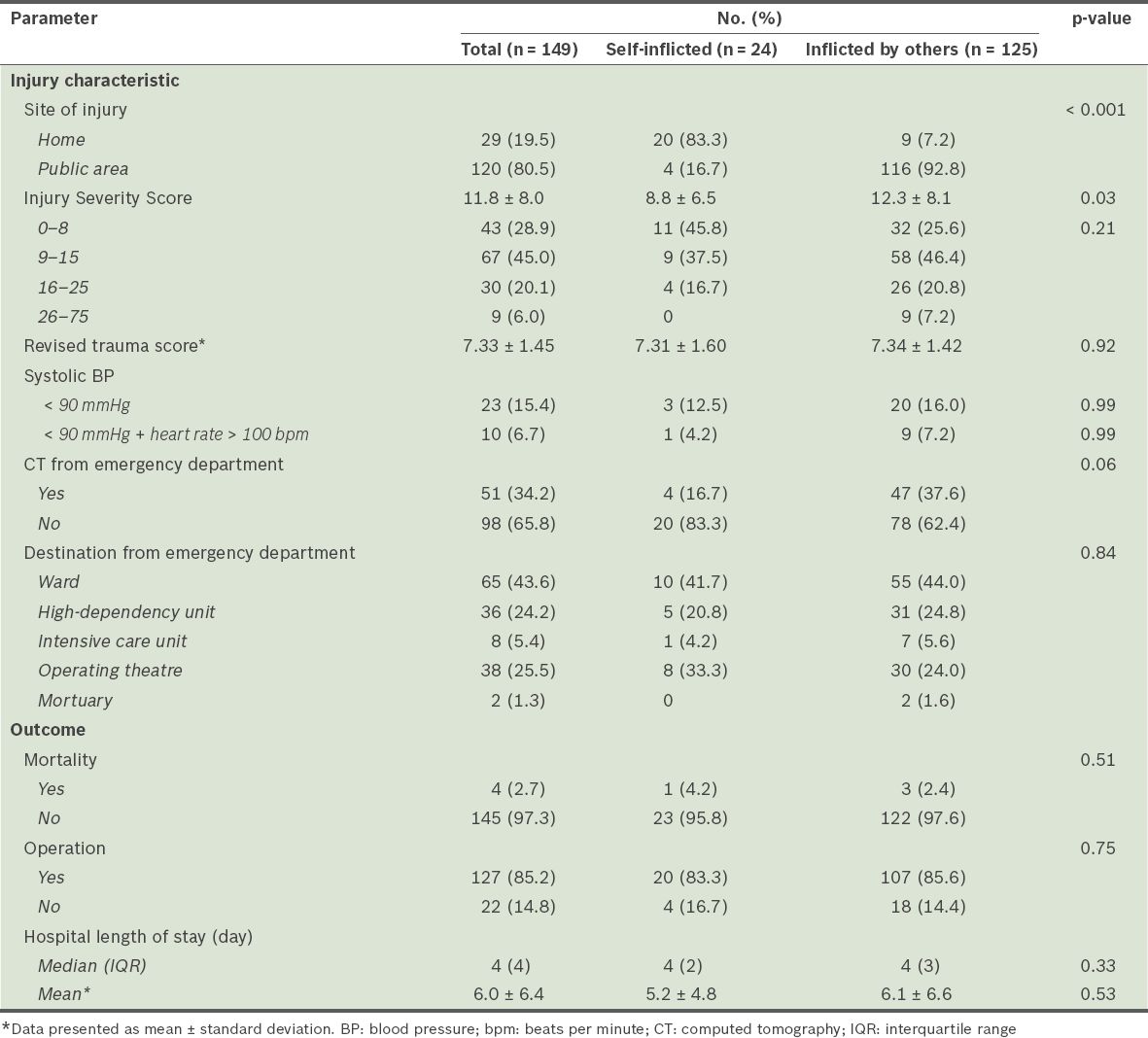
In terms of disposition from the ED, 4 (16.7%) from the SI group required further imaging evaluation via computed tomography (CT), as opposed to 47 (37.6%) from the IO group (p = 0.06). There were no observed differences in the patients’ destinations from the ED, whether it was the general ward, high-dependency or intensive care units, or the operating theatre. Two patients in the IO group died in the ED and were sent to the mortuary. Most patients in both the SI and IO groups required an operation (83.3% vs. 85.6%). Mortality rates in both groups were similarly low (n = 1, 4.2% vs. n = 3, 2.4%; p = 0.51). The median hospital LOS in the SI and IO groups were similar at 4 (interquartile range [IQR] 2) and 4 (IQR 3) respectively (p = 0.33) (
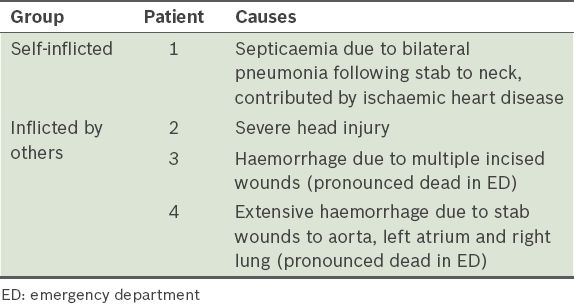
The causes of death in these stab wound cases are summarised in
Table III
Causes of death in patients with stab wound injuries.
DISCUSSION
Our study found that stab wound victims are likely to be young men (
Our study found that patients in the IO group had significantly higher ISS scores than those in the SI group (
Despite differences in injury severity, patients in both groups achieved similar outcomes in terms of mortality rates and hospital LOS (
Our study has provided an epidemiologic profile of the types of stab wound injuries in Singapore. A mortality risk is present for all penetrating stab wound injuries, with the area of injury (e.g. head and neck, anterior chest, etc) being the most important factor in the management of patients. When penetrating injuries traverse anatomic regions (e.g. chest into abdomen cavity), they are also likely to be more severe. Such pertinent clinical information, which clinicians have been trained to utilise according to Advanced Trauma Life Support principles, together with our proposed categorisation of the stab wound (i.e. SI or IO), can help clinicians to better profile trauma patients in a safe and rational manner. In a crowded emergency room, the senior clinician in charge must perform the initial assessment, especially when a penetrating injury is deemed to be IO. Our findings are congruent with data from a 2001 survey of fatal and non-fatal injuries in the United States, where case fatality rates of unintentional injuries (e.g. fall, motor vehicle accident and self-harm) were 0.37, compared to 1.12 for intentional injuries (e.g. from gunshots).(9) Due to our low numbers (n = 4), we cannot demonstrate that intent of injury is an important determinant of trauma mortality outcomes in our study; however, injury severity has long been recognised to be strongly associated with trauma mortality.(10) Compared to other cohort studies investigating stab wound injuries, our study is similar in terms of injury severity. A 12-year study of abdominal stab wound injuries at Cedars-Sinai Medical Center in Los Angeles, California,(11) found that of 249 stab wound injuries, the mean ISS was 11.1 ± 7.9, similar to that of the current study (11.8 ± 8.0). The use of CT was 35.0%, which is comparable to that in the current study (34.2%), and the operative rate was 83.3% vs. 85.2% in our study, suggesting that our trauma centre has similar practice patterns to an urban Level 1 trauma centre in the US.
Our study should be interpreted in light of the following limitations. Firstly, this was a retrospective cohort study. Secondly, this data represents the experience from a single centre and may not be nationally representative. Thirdly, we did not have reliable data available to assess alcohol intoxication (i.e. blood alcohol level), hence could not evaluate if this was a contributory factor to these patients’ stab wound injuries.(12) Furthermore, we did not have further descriptive data on the injuries, such as type of weapon used, number of times a patient was stabbed and where they were stabbed (e.g. which quadrant in the abdomen), as this data was either not available at the patient’s presentation to the ED or not electronically available. Lastly, we were also unable to evaluate if patients were subsequently re-admitted to another tertiary hospital for similar self-risking behaviour. Further research to track the outcomes of the SI patients (e.g. details of follow-up appointments at specialist outpatient clinics) may be valuable in characterising the profile of this special group of patients,(13-15) especially as patients with a previous deliberate self-harm episode have a 30-fold increase in risk of suicide compared with the general population.(16)
CONCLUSION
Our retrospective review study confirms our hypothesis that SI injuries are indeed less severe than IO injuries, based on ISS and proportion of patients presenting with circulatory shock. However, this did not translate into differences in mortality or hospital LOS outcomes. This study adds to our understanding of the nature of stab wound injuries and can help guide trauma services in triage and management.
ACKNOWLEDGEMENTS
We would like to thank the late Mr A Vijayan, Senior Consultant, and Mr Chua Wei Chong, Consultant, Trauma Services, Department of General Surgery, Tan Tock Seng Hospital, for their contributions in allowing us to use data collected from their patients for this study.


