Abstract
INTRODUCTION
The study aimed to determine the prevalence and documentation of delirium among the elderly and if the Clock Drawing Test (CDT) can be used to predict which patients had delirium on admission and those who may develop delirium during their stay in acute medical wards.
METHODS
A single researcher performed the Mini-Mental State Examination (MMSE) and CDT on admission and discharge of 57 elderly adults at the National University Hospital, Singapore. Delirium was defined as a ≥ 3-point improvement or ≥ 2-point decline in MMSE scores from admission to discharge, where a fall denotes development of delirium and a rise denotes resolution. The case notes of the same patients were reviewed for documentation of delirium. All inpatients from two acute medical wards were examined. One CDT score and a pair of MMSE scores were collected from each patient.
RESULTS
A total of 57 patients (28 male, 29 female) were involved in the study. Their mean age was 76.0 ± 8.7 years. The prevalence of delirium based on MMSE scores was 40.4%; 16 patients had delirium on admission while seven developed delirium during their inpatient stay. However, delirium was documented in the case notes of only 7 (30%) of the 23 patients. CDT score was better than baseline MMSE score at predicting a decline in MMSE score.
CONCLUSION
The prevalence of delirium in the acute medical setting is high but underdiagnosed. The CDT may be a good screening tool to identify patients at risk of delirium during their inpatient stay. Baseline cognition screening should be performed in every elderly patient admitted to hospital.
INTRODUCTION
Delirium, defined by O’Keeffe as a ≥ 3-point improvement or ≥ 2-point decline in Mini-Mental State Examination (MMSE) scores from admission to discharge, where a fall denotes development of delirium and a rise denotes resolution,(1) is a reversible mental disorder that is often caused by multiple factors.(2,3) Proper identification and treatment can prevent increased healthcare costs,(4-6) prolonged hospital stay(5) and increased likelihood of placement in a nursing home on discharge.(7,8) Studies on delirium conducted in the hospital setting have found that it is the single most common acute mental disorder among hospitalised elderly patients.(9-11) Prospective studies of medical inpatients in Western countries reported a prevalence of delirium (i.e. existing cases on hospital admission) of 12%–31%(12,13) and incidence rates (i.e. new cases arising during the hospital stay) of 3%–25%.(5,14) It has also been reported that about 30% of elderly patients experience delirium at some time during hospitalisation.(15,16) Despite its frequent occurrence and significant consequences, delirium is often underrecognised. It is not detected by healthcare personnel in up to 70% of patients(17) and is often unrecognised on hospital admission.(18)
We hypothesised that the primary team often misses the diagnosis of delirium when managing elderly patients admitted to the acute medical ward. This study aimed to determine the prevalence and rate of underreporting of delirium among elderly patients admitted to the acute medical wards of a tertiary hospital in Singapore, and to compare the ability of two cognitive screening tests, the MMSE and the Clock Drawing Test (CDT), to predict the development or resolution of delirium during hospitalisation.
METHODS
A single researcher conducted the MMSE and CDT for 57 patients aged ≥ 60 years who were admitted to two acute medical wards in the National University Hospital, Singapore, in June 2011 and June 2012. The MMSE was performed within 24 hours of admission and discharge, and the CDT was performed within 24 hours of admission. Patients were excluded if they were uncommunicative, had a severe hearing impairment or were discharged within 24 hours of admission.
The MMSE is a 20-item test that screens for cognitive impairment.(1,19) It has a total score of 30 points. The items are clustered into 11 subscores measuring orientation to time (maximum possible score [max] 5), orientation to location (max 5), immediate recall (max 3), attention and calculation (max 5), delayed recall (max 3), naming (max 2), verbal repetition (max 1), ability to follow a three-stage command (max 3), reading (max 1), writing (max 1) and figure-copying (max 1). Cognitive impairment was defined using MMSE scores and education-adjusted cutoffs(20) of < 21 points for patients with < 6 years of education, < 23 points for patients with 6–12 years of education and < 24 points for patients with > 12 years of education (
For the CDT, we used the scoring method adapted by Shulman et al from Cahn et al.(21-24) The instructions given to the patients and scoring system used (range 1–5, with 5 being normal) are shown in
Demographic and clinical characteristics of the patients that involved categorical variables were summarised using counts and percentages. For continuous variables, mean and standard deviation were used to describe the data distribution. The primary outcome variable was the development or resolution of delirium during hospitalisation and was based on O’Keeffe et al’s definition of either (a) an improvement in MMSE score by ≥ 3 points to detect resolution of delirium; or (b) decline in MMSE score by ≥ 2 points from admission to discharge to detect development of delirium.(1) A change in MMSE score between –1 and +2 is considered equivocal. We used the chi-square test to examine the association between cognitive status on admission (measured by MMSE/CDT score) and change in MMSE score on discharge, as well as the association between change in MMSE score on discharge and re-admission rates up to three months after discharge. We examined the independent associations of CDT and MMSE scores at admission compared to change in MMSE score on discharge using logistic regression. All statistical analyses were generated using IBM SPSS Statistics version 20.0 (IBM Corp, Armonk, NY, USA), using a two-sided test at a 5% level of significance.
RESULTS
A total of 57 pairs of MMSE scores were collected from 28 (49%) male and 29 (51%) female patients. Their mean age was 76.0 ± 8.7 years and the mean length of hospital stay was 6.0 ± 3.3 days. On admission, 26 (46%) of the 57 patients had MMSE scores within the normal range, while 31 (54%) patients had impaired MMSE scores (
Table I
Summary of changes in Mini-Mental State Examination (MMSE) scores on discharge and case note documentation on the patients (n = 57).
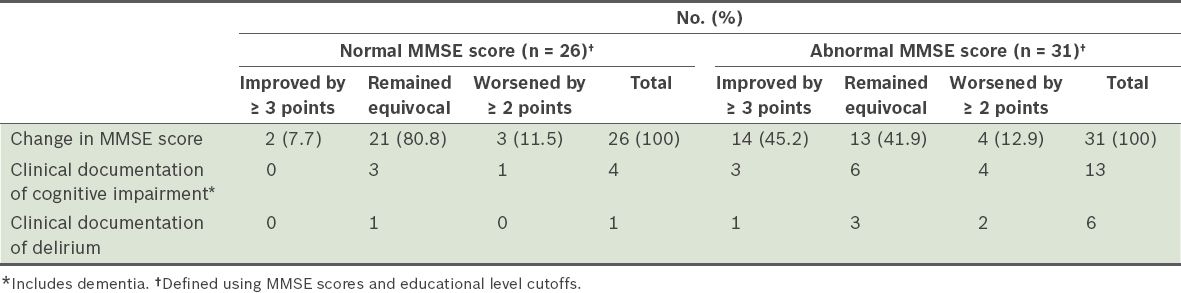
On discharge, regardless of their cognitive state on admission, the MMSE scores of 16 (28.1%) patients had an improvement of ≥ 3 points and 7 (12.3%) patients had a decline of ≥ 2 points (
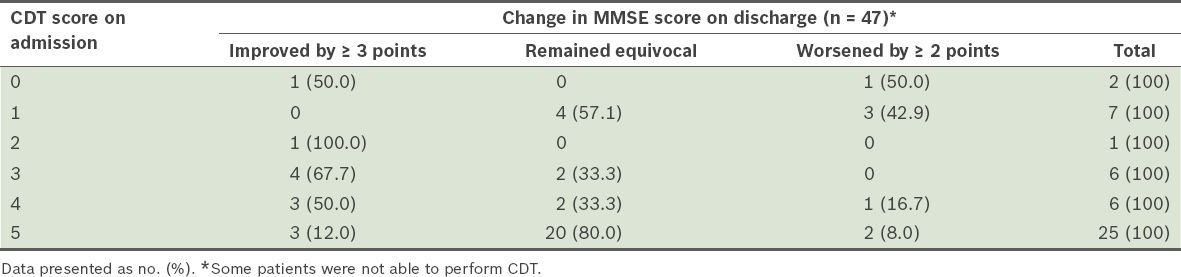
Among the 16 patients who had a CDT score of 0–3 points on admission, 4 (25.0%) worsened by ≥ 2 points, 6 (37.5%) remained equivocal and 6 (37.5%) improved by ≥ 3 points in their MMSE scores on discharge (
Table II
Relationship between Clock Drawing Test (CDT) score on admission and change in Mini-Mental State Examination (MMSE) score on discharge.
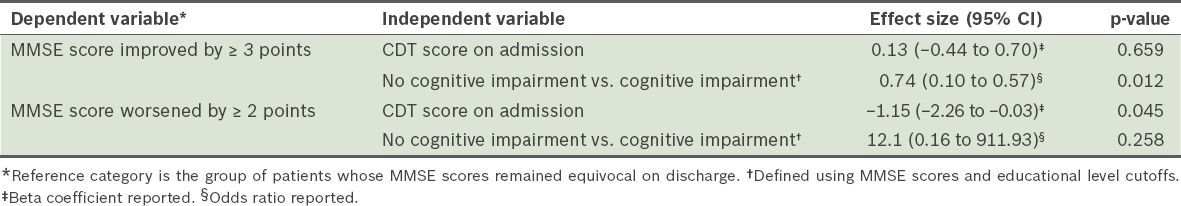
Logistic regression analysis adjusted for age, gender and ethnicity showed that normal cognition, assessed according to the patient’s MMSE score on admission, was a predictor of absence of delirium or resolution of delirium during the hospital stay, i.e. an equivocal change in MMSE score (odds ratio [OR] 0.74, 95% confidence interval [CI] 0.10 to 0.57, p = 0.012). CDT score on admission in itself was not a predictor of delirium during the hospital stay (ß = 0.13, 95% CI −0.44 to 0.70, p = 0.659) (
Table III
Comparison of Mini-Mental State Examination (MMSE) and Clock Drawing Test (CDT) scores at admission predicting improvement in cognition on discharge.
DISCUSSION
In our study, the prevalence of delirium was 28.1% on admission to the acute medical ward and 12.3% of the patients developed delirium during their stay. This is comparable with international data from well-established hospitals, which showed that the prevalence of delirium in medical inpatients on admission was between 12% and 31%,(12,13) and the development of delirium during admission was 3%–25%.(5,14) However, less than one-third of the patients who had delirium in the present study were documented to have this condition, suggesting that delirium is often overlooked in the day-to-day care of elderly patients admitted to acute medical wards. Previous studies have found that delirium is overlooked in up to 68% of patients.(27) It has been reported that untreated delirium increases mortality rates up to three-fold, increases the chance of discharge to nursing home and increases long-term cognitive impairment by up to ten times.(5,12,28,29) As age is a major predisposing factor for delirium, failing to diagnose delirium will increase the economic burden of caring for elderly patients in Singapore’s ageing population.
Our study also showed that a normal MMSE score at admission was a better predictor than the CDT score of the absence of delirium during hospitalisation. On the other hand, a lower CDT score was better than the MMSE score in predicting patients whose MMSE score would worsen on discharge. Our findings suggest that the CDT is a good screening tool to detect those at high risk of developing delirium during their inpatient stay. However, this finding should be confirmed by a larger study using a gold-standard diagnostic tool for delirium, such as the Confusion Assessment Method.(8)
The strength of this pilot study was that the data was collected by a single researcher, hence reducing random error and interviewer bias. Its limitations were the small sample size and lack of correlation with the use of catheters and restraints, anticholinergic burden of medications in patients, and underlying function or principal diagnosis for admission. In addition, the correlation between these methods of measuring cognitive changes and the Confusion Assessment Method was not assessed. The test-retest reliability of the MMSE as a screening tool may also be a concern; however, studies have shown that the amount of change in MMSE score was small, usually less than 2 points.(30) Another major limitation of the study is that MMSE scores could have remained equivocal (i.e. did not change) for the patients who were delirious at admission and remained so at discharge.
Our study confirmed that the prevalence of delirium is 40% among older adult inpatients admitted to acute medical wards, and that delirium was overlooked in 70% of these patients. Interestingly, we found that the CDT is better at predicting patients who will develop delirium during their inpatient stay than the baseline MMSE. We found no statistical difference in terms of length of stay and re-admission rates between those with normal or impaired MMSE scores. As delirium is often overlooked by medical professionals but is an important prognostic indicator, all older adults admitted to acute hospitals should be screened for underlying cognitive impairment and delirium. Further larger-scale studies are required to evaluate if the CDT can be used as a screening tool to identify older adults at risk of developing delirium in hospitals.
ACKNOWLEDGEMENTS
The authors would like to thank A/Prof Tai Bee Choo and Mr Benjamin Er from the Saw Swee Hock School of Public Health, National University of Singapore, Singapore, for advising in statistical analysis for this paper.


