Abstract
Chronic cough is one of the most common reasons for referral to a respiratory physician. Although fatal complications are rare, it may cause considerable distress in the patient’s daily life. Western and local data shows that in patients with a normal chest radiograph, the most common causes are postnasal drip syndrome, postinfectious cough, gastro-oesophageal reflux disease and cough variant asthma. Less common causes are the use of angiotensin-converting enzyme inhibitors, smoker’s cough and nonasthmatic eosinophilic bronchitis. A detailed history-taking and physical examination will provide a diagnosis in most patients, even at the primary care level. Some cases may need further investigations or specialist referral for diagnosis.
Wendy, a successful executive in her early 30s, visited your clinic for a review. She complained that her prolonged cough was irritating her, particularly at work. She described a dry cough with occasional whitish phlegm and a slight itch in the throat, which was especially prevalent when she had to do a long presentation.
WHAT IS CHRONIC COUGH?
In common practice, any non-acute cough (≥ 3 weeks’ duration) is considered 'chronic'. However, international guidelines subdivide non-acute cough into subacute (3–8 weeks duration) and chronic (> 8 weeks duration).(1) Studies have suggested that only a small proportion of those affected by chronic cough present themselves for medical attention,(2) and those who attend consultations may report experiencing significant distress or a reduced quality of life as a result of their cough.(3) However, for the purpose of this article, we will focus on the common presentations and use the term ‘chronic’ for any prolonged cough lasting ≥ 3 weeks.
HOW COMMON IS THIS IN MY PRACTICE?
According to the Ministry of Health Primary Care Survey 2010, cough (of varying durations) is the most common presentation, appearing in up to 25% of all general practitioner and polyclinic attendances.(4) Chronic cough is one of the most common indications for referral to a pulmonary specialist. However, careful history-taking and physical examination at the primary care level can narrow the diagnosis in many of these patients. Chronic cough is rarely life-threatening, but serious complications like pneumothorax, syncope and cardiac arrhythmias can sometimes occur.
WHAT CAN I DO IN MY PRACTICE?
The article mainly focuses on (a) adult patients; (b) who present with cough as the primary symptom; (c) when the cough is not associated with fever, dyspnoea, weight loss or any other warning symptoms; and (d) who have a normal chest radiograph. In this group, common causes are postinfectious cough, cough variant asthma (CVA), postnasal drip syndrome (PNDS), gastro-oesophageal reflux disease (GERD), smoker’s cough, use of angiotensin-converting enzyme inhibitors (ACEI) and nonasthmatic eosinophilic bronchitis (NAEB).
What are some typical features of these differentials?
Postinfectious cough
This cough usually follows a viral upper respiratory tract infection and spontaneously subsides within eight weeks (subacute cough). The aetiology is believed to be transient laryngeal hyperresponsiveness.
Mycoplasma and pertussis have both been associated with postinfectious cough in adults. Mycoplasma cough usually lasts for 1–2 months and may be associated with high serum Mycoplasma titres. There is no evidence that antibiotics have any benefits in treating this cough. Pertussis, which is also known as 100-day cough or whooping cough, is increasingly seen in adults (including those who were immunised in childhood) and may last up to four months. As these patients do not usually display the typical features of pertussis, a prolonged cough may be the only main symptom. In most patients, the cough does not have a 'whooping' quality. While macrolides or doxycycline may reduce the risk of transmission, they probably have little effect on the cough itself.
Cough variant asthma
CVA is asthma presenting mostly as cough, with little or no dyspnoea. The cough may be 'wheezy' in nature. These patients sometimes present with normal spirometry and a methacholine challenge test (MCT) may be needed for diagnosis. A negative MCT essentially rules out CVA. Once confirmed, patients with CVA respond well to standard asthma therapy, such as inhaled corticosteroids.
Postnasal drip syndrome
PNDS is now referred to as upper airway cough syndrome and is caused by chronic rhinitis (allergic and nonallergic) or chronic sinusitis. Patients usually present with a runny or blocked nose, nasal dripping, and an itchy throat. Purulent discharge and facial pain may suggest concomitant sinusitis. A careful physical examination of the posterior oropharyngeal space may reveal a cobblestone appearance. Allergic rhinitis will usually respond to antihistamine treatment and a course of at least two weeks of nasal steroids. However, longer-term treatment may be required for the control of persistent allergic rhinitis, which is commonly found in Singapore. If the cough does not resolve and chronic sinusitis is suggested, the patient should be referred to an ear, nose and throat physician for further investigations and management.
Gastro-oesophageal reflux disease
Patients experiencing this may present with classical symptoms such as acid brash, heartburn and bloating. A therapeutic trial with acid-suppressive medication, such as proton pump inhibitors, with or without promotility agents may be started. However, some patients have atypical presentations that may be due to non-acid reflux. These patients may need more specialised investigations, including upper gastrointestinal endoscopy, 24-hour pH monitoring or gastric impedance testing.
Smoker’s cough
Heavy smokers can develop chronic bronchitis, generally after 40 years of age. This is classically a 'wet' cough with white, tenacious sputum and tends to occur in the morning.
Cough following use of angiotensin-converting enzyme inhibitors
Following the start of ACEI therapy, cough may be seen in up to one-third of these patients. This cough may appear immediately or as late as a few months into the therapy. Resolution of the cough usually occurs 2–4 weeks after cessation of the offending drug, although some cases may take a few months to resolve. A study from Tampines Polyclinic revealed a 30% incidence of post-ACEI cough; the majority of the affected patients were successfully switched to angiotensin receptor blockers.(5)
Nonasthmatic eosinophilic bronchitis
NAEB is identified in patients as eosinophilic inflammation of the airway without bronchospasms and is often associated with sputum eosinophilia. Lung function tests such as spirometry and MCT return normal results. Patients respond well to inhaled corticosteroids.(6,7)
How can I approach chronic cough?
Unpublished local data on 200 consecutive cases of chronic cough assessed by Poulose et al showed that the most common causes referred to a respiratory clinic at Changi General Hospital, Singapore, were PNDS, postinfectious cough, GERD and CVA. A diagnosis could not be reached in 21 (11%) patients. These cases included 12 patients who were lost to follow-up after the first visit. In 20% of cases, more than one aetiology was identified.
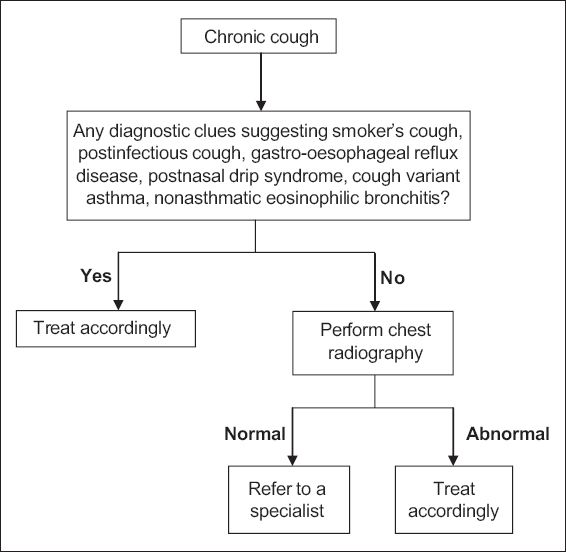
When approaching a case of chronic cough, proper history-taking is of paramount importance. Many of the referred cases in our local data were diagnosed at the first visit through the patients’ detailed history alone (including four cases of smoker’s cough). Other cases may present with no diagnostic clues, even after a detailed history-taking, physical examination and chest radiography. A study conducted in Singapore by Poulose et al(8) on such cases showed that in 65% of them, a diagnosis was eventually reached. The most common aetiologies were GERD and PNDS.(8) A suggested approach to chronic cough is given in
Fig. 1
Flowchart shows suggested approach to chronic cough.
WHEN SHOULD I REFER TO A SPECIALIST?
In healthcare settings in which there is no easy access to specialist care, the primary care physician may order further investigations when there are no clear diagnostic clues. An alternative approach is to try empiric treatment (a therapeutic trial) for the most common causes of chronic cough (i.e. GERD, PNDS and CVA). However, the treatment period of such empiric trials may last up to a few months and the uncertainty of success may cause patients further anxiety.
In the local context, where the specialist referral system is more efficient, we recommend referring the patient (
After a careful history-taking, you found out that Wendy started out with an upper respiratory tract infection with rhinorrhoea and sore throat. These resolved in the first few days after presentation and only the dry cough persisted. Her physical examination was normal. You explained to Wendy that her cough was a common presentation after an infection of the upper airway, as its natural course is 4–8 weeks, and prescribed her another course of cough syrup. You received a 'Thank you' card from Wendy about two weeks later, informing you that her cough had completely resolved.
TAKE HOME MESSAGES
-
The most common causes of chronic cough, in the local context, appear to be PNDS, postinfectious cough, GERD and CVA.
-
Postinfectious cough usually follows a viral upper respiratory tract infection and may last up to eight weeks.
-
A careful history-taking and physical examination can provide a diagnosis in many patients.


