Abstract
The Ministry of Health (MOH) has developed the clinical practice guidelines on Prevention, Diagnosis and Management of Tuberculosis to provide doctors and patients in Singapore with evidence-based treatment for tuberculosis. This article reproduces the introduction and executive summary (with recommendations from the guidelines) from the MOH clinical practice guidelines on Prevention, Diagnosis and Management of Tuberculosis, for the information of SMJ readers. The chapters and page numbers mentioned in the reproduced extract refer to the full text of the guidelines, which are available from the Ministry of Health website:
INTRODUCTION
Tuberculosis continues to be a disease of public health importance in Singapore and worldwide. According to the World Health Organisation’s Global Tuberculosis Report 2014, an estimated 9 million people developed tuberculosis and 1.5 million died from the disease. Issues like delayed detection and missed opportunities for treatment, and the emergence of drug-resistance are also of increasing concern.
1.1 Aim
The target audience is all healthcare practitioners in Singapore. These guidelines aim to:
Increase knowledge and awareness of tuberculosis so as to facilitate the early detection of active tuberculosis.
Serve as an evidence-based resource to provide guidance on the use of tuberculosis diagnostic tools and treatment regimens.
Inform regarding the public health measures necessary for the control of tuberculosis control in Singapore.
1.2 Scope
These guidelines will cover tuberculosis referral and diagnosis, treatment of active and latent tuberculosis, and public health actions required on the part of treating physicians. The standards of diagnosis and treatment, which are outlined in the International Standards for Tuberculosis Care, will also be referenced in the clinical practice guidelines (CPG).
1.3 Target group
The content of the guidelines will be useful for all healthcare professionals and public health service providers who encounter patients with tuberculosis. The CPG will be applicable to the diagnosis and management of both adult and paediatric patients. The doctor evaluating the patient is ultimately responsible for clinical decisions made after reviewing the individual patient’s history, clinical presentation and treatment options available.
1.4 Development of guidelines
These guidelines have been produced by a committee of respiratory physicians, infectious disease consultants, and representatives from polyclinics and the College of Family Physicians Singapore, as well as representatives from Ministry of Health (MOH) and Tuberculosis Control Unit appointed by the MOH. They were developed by the adaptation of existing guidelines, by the review of relevant literature and by expert clinical consensus with consideration of local practice.
The following principles underlie the development of these guidelines:
Treatment recommendations are supported by scientific evidence and expert clinical consensus.
Treatment should maximise therapeutic and public health benefits and minimise side effects.
1.5 Review of guidelines
Evidence-based CPGs are only as current as the evidence that supports them. Users must keep in mind that new evidence could supersede recommendations in these guidelines. The workgroup advises that these guidelines be scheduled for review five years after publication, or when new evidence appears that requires substantive changes to the recommendations.
EXECUTIVE SUMMARY OF RECOMMENDATIONS
Details of recommendations can be found on the indicated pages. Key recommendations are highlighted in grey.
Tuberculosis Transmission and Pathogenesis
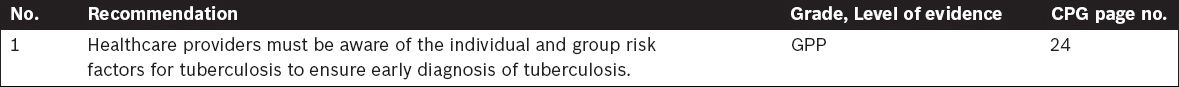
Clinical Diagnosis of Tuberculosis
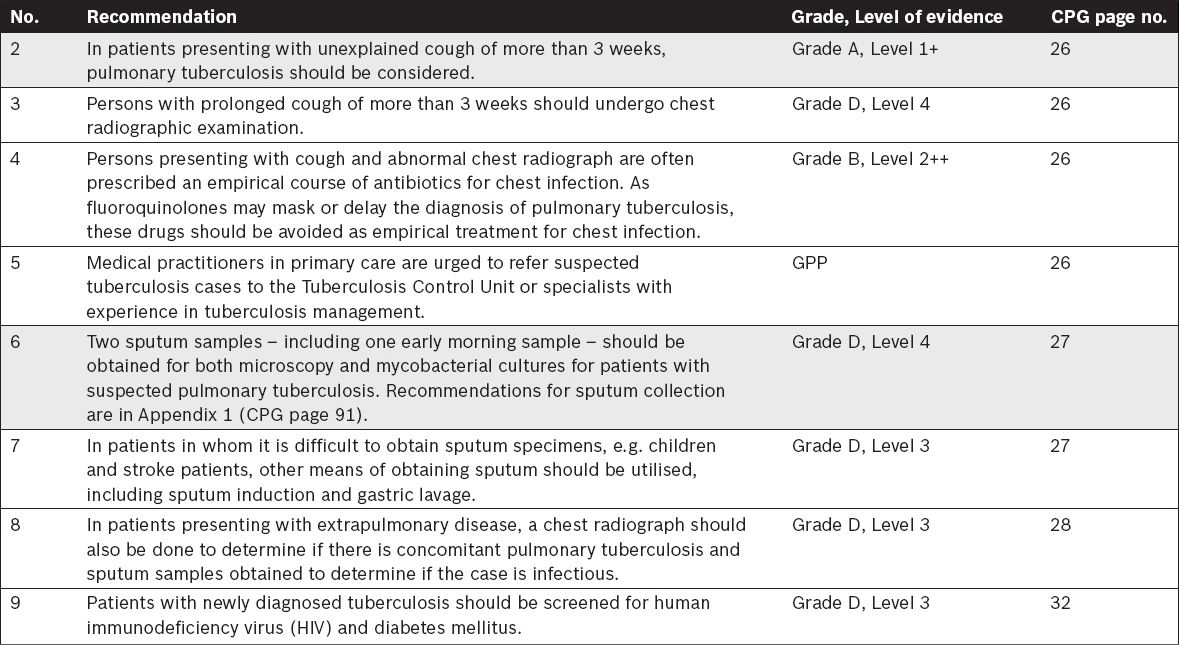
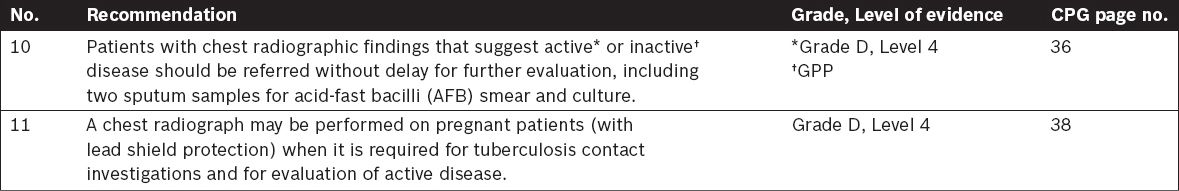
Imaging in Tuberculosis
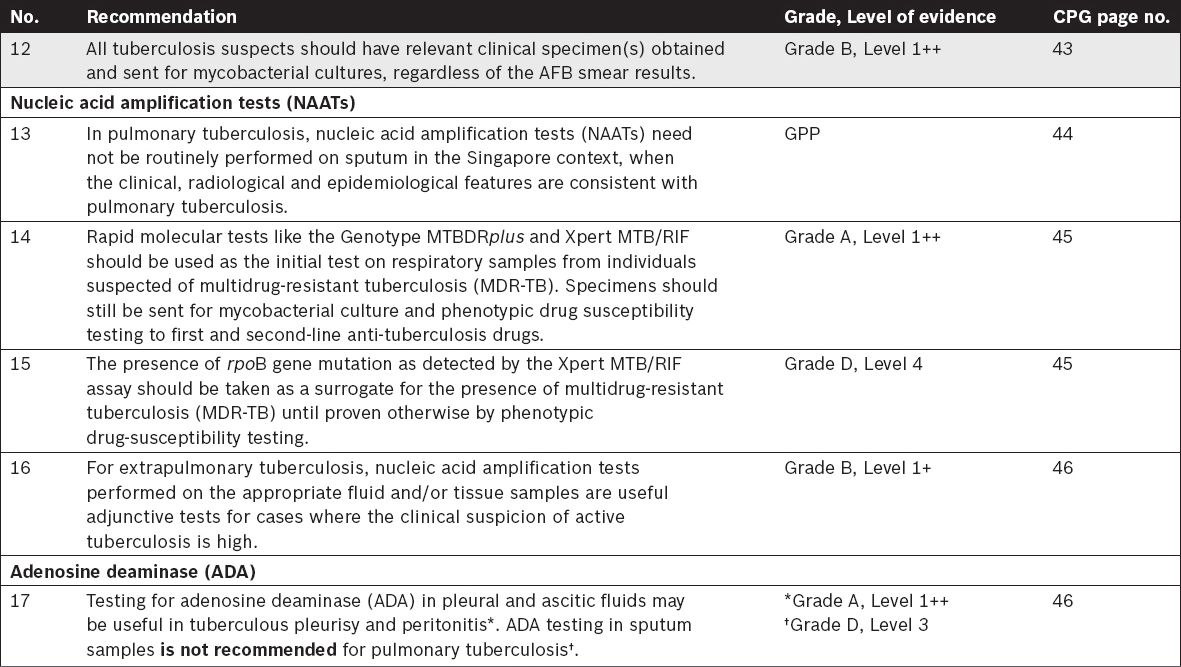
Tuberculosis Laboratory Diagnosis
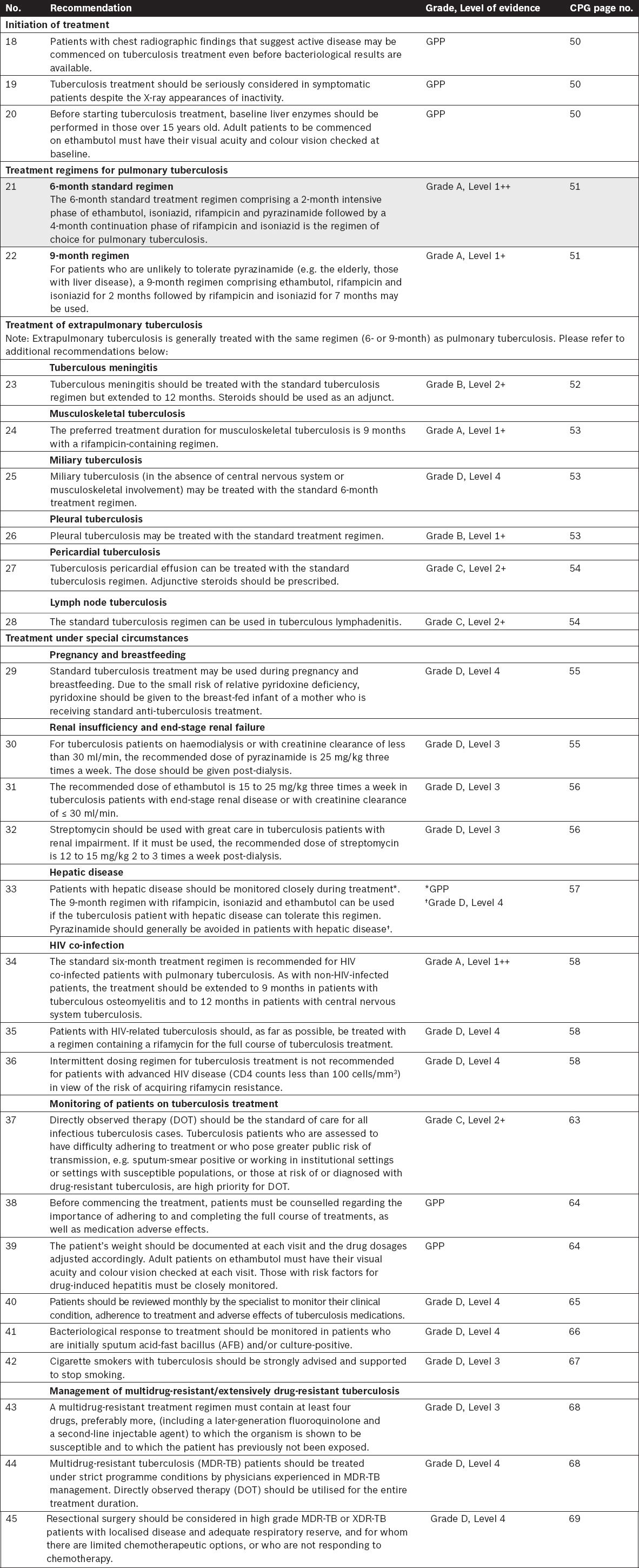
Treatment of Tuberculosis
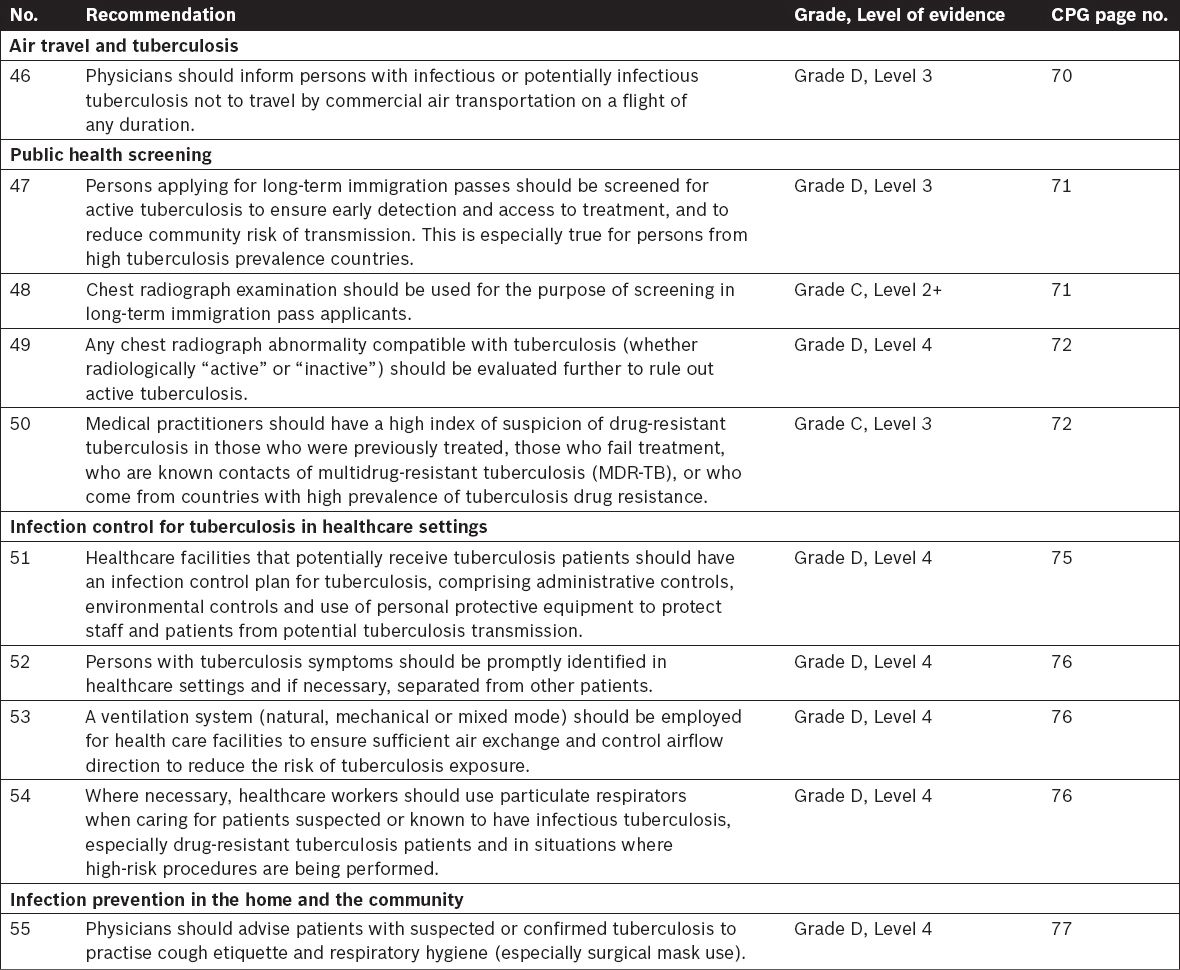
Public Health Screening and Infection Control
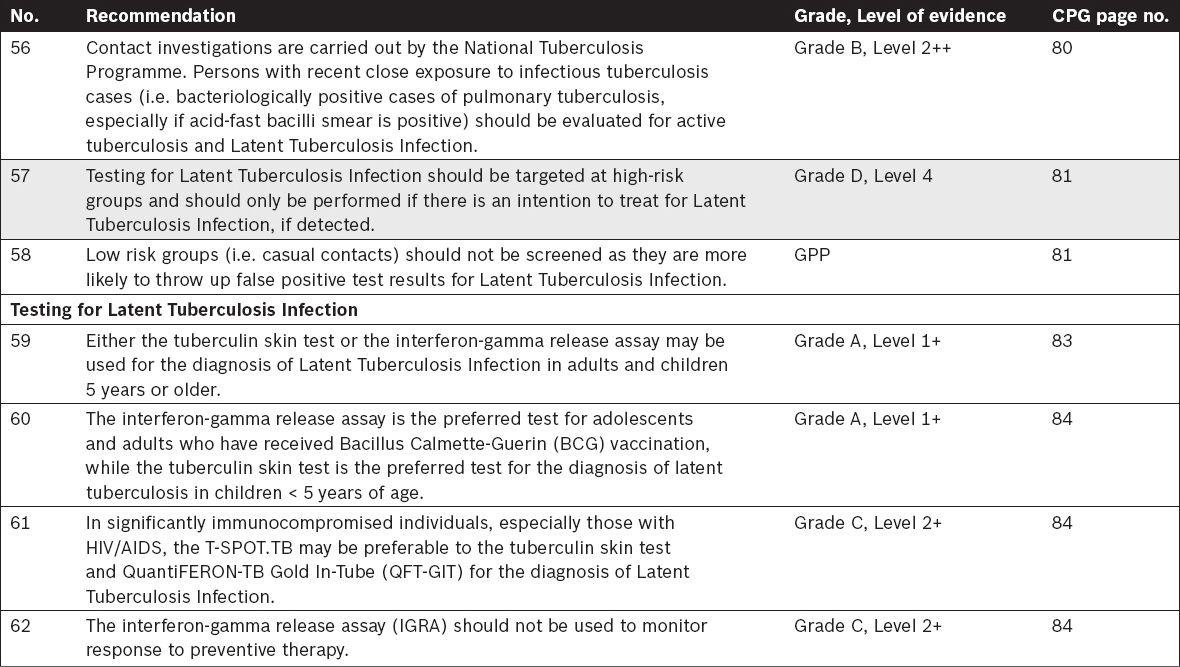
Tuberculosis Contact Investigations and Screening
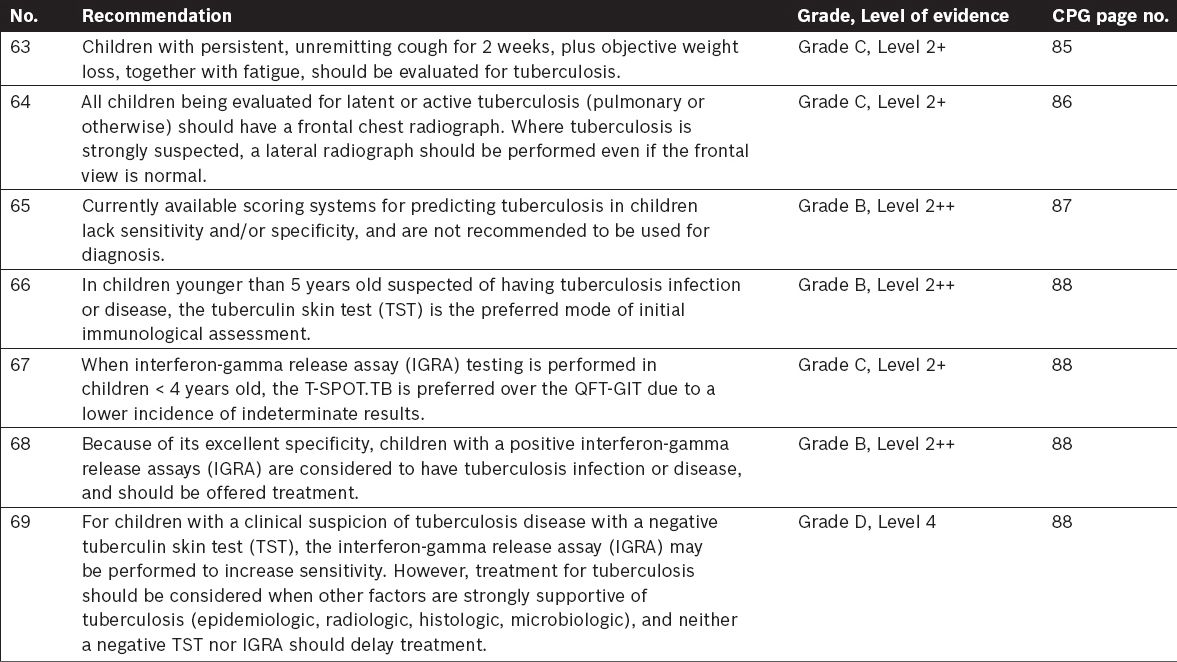
Tuberculosis in Children – Specific Considerations
SMJ-57-124-appendix.pdf
SMJ-57-125.pdf


