Abstract
Secondary hypertension occurs in a significant proportion of adult patients (~10%). In young patients, renal causes (glomerulonephritis) and coarctation of the aorta should be considered. In older patients, primary aldosteronism, obstructive sleep apnoea and renal artery stenosis are more prevalent than previously thought. Primary aldosteronism can be screened by taking morning aldosterone and renin levels, and should be considered in patients with severe, resistant or hypokalaemia-associated hypertension. Symptoms of obstructive sleep apnoea should be sought. Worsening of renal function after starting an angiotensin-converting enzyme inhibitor suggests the possibility of renal artery stenosis. Recognition, diagnosis and treatment of secondary causes of hypertension lead to good clinical outcomes and the possible reversal of end-organ damage, in addition to blood pressure control. As most patients with hypertension are managed at the primary care level, it is important for primary care physicians to recognise these conditions and refer patients appropriately.
Mr Ali, aged 55 years, visited you for a scheduled follow-up for his hypertension, Type 2 diabetes mellitus, ischaemic heart disease and a prior ischaemic stroke. Your first consultation with him was two weeks ago, when he transferred his medical follow-up to your clinic. You reviewed his medications and noted that he is currently taking five antihypertensive medications (hydrochlorothiazide, hydralazine, enalapril, atenolol and amlodipine). His blood pressure during the visit was 154/96 mmHg, while his blood pressure recorded at home was generally about 150/90 mmHg or higher. You reviewed his first set of blood investigations at your clinic and noted that he has hypokalaemia (serum potassium 3.0 mmol/L).
WHAT IS SECONDARY HYPERTENSION?
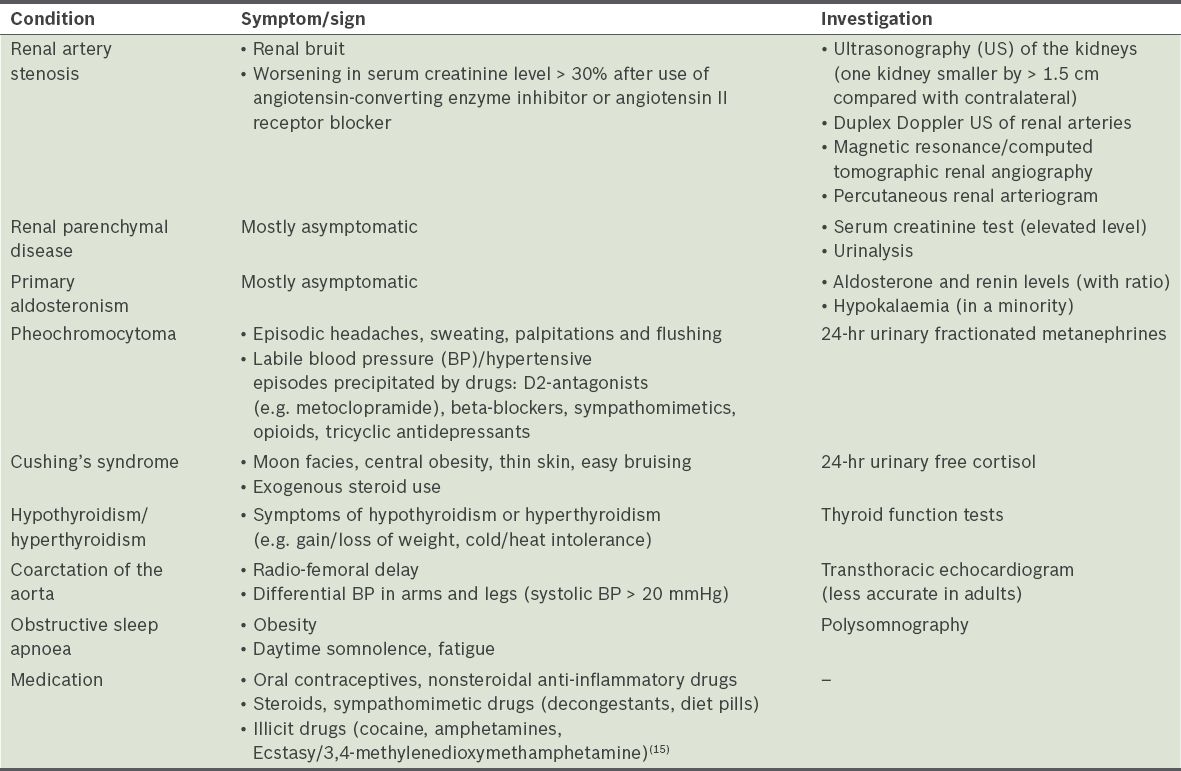
Hypertension is the single biggest contributor to the global burden of disease,(1) and is the most common chronic medical condition presenting to primary care physicians in Singapore.(2) While the majority of patients have essential hypertension that does not have an identifiable cause, it is important to recognise secondary causes of hypertension (
Table I
Causes of secondary hypertension and suggestive findings.
HOW COMMON IS THIS IN MY PRACTICE?
About 10% of patients with hypertension have a secondary cause. Clinicians often consider secondary causes such as renal disease or coarctation of the aorta in children and young adults aged below 30 years. However, it is important to realise that secondary causes are also common in older patients, particularly primary aldosteronism, renal disease and obstructive sleep apnoea (OSA). The prevalence of these conditions is even higher in patients with resistant hypertension, defined as blood pressure (BP) ≥ 140/90 mmHg despite the use of three antihypertensive medications, including a diuretic.(3-6) Other causes, such as pheochromocytoma, are less common but equally important to recognise, as failure to diagnose and treat them can lead to catastrophic consequences.(7)
WHAT CAN I DO IN MY PRACTICE?
The diagnosis of hypertension should be confirmed with at least two BP readings (≥ 140/90 mmHg) using a mercury sphygmomanometer or another noninvasive device at two separate settings. Following this, a directed history and physical examination should be performed to consider secondary causes of hypertension; this should always include an evaluation for other cardiovascular risk factors, including diabetes mellitus, hyperlipidaemia, family history and smoking status.
Important clues suggesting an underlying secondary cause are (a) young patient < 30 years of age (renal causes or coarctation of the aorta); (b) symptoms or signs suggesting secondary causes (
Primary aldosteronism
First described by Jerome Conn in 1950, primary aldosteronism (PA) was thought to be rare (< 1%) and that hypokalaemia was a sine qua non.(8) However, more sensitive laboratory assays and the use of the aldosterone-to-renin ratio (ARR) as a screening test has led to an increase in diagnosis of PA worldwide.(9) It is currently well-recognised that only a minority of patients (~30%) have hypokalaemia.(5) One local polyclinic study screened and confirmed PA in 5% of hypertensive patients,(4) while another study at a local tertiary centre found a prevalence of 13% in diabetic patients with resistant hypertension.(3) It is important to diagnose these patients, as they often have increased cardiovascular morbidity and mortality than age-, sex- and BP-matched patients with essential hypertension,(10) and treatment can lead to reversal of end-organ damage.(11-14) Surgery is usually recommended for patients with a unilateral adrenal adenoma (termed Conn's syndrome), while patients who have bilateral adrenal hyperplasia or who are not suitable for or keen on surgery are treated with mineralocorticoid receptor antagonists (spironolactone or eplerenone). Surgery improves BP in all patients, and hypertension is cured in about 50% of patients.(5)
Patients with PA are often aged about 50–70 years; only a minority have hypokalaemia and almost all are asymptomatic.(3,4,9) Hence, it is important to consider screening patients for this condition. The Endocrine Society in the United States released a guideline(5) in March 2016 recommending broadened indications for screening of PA in patients with hypertension (
Table II
Screening for primary aldosteronism (adapted from the Endocrine Society Guidelines 2016).(5)
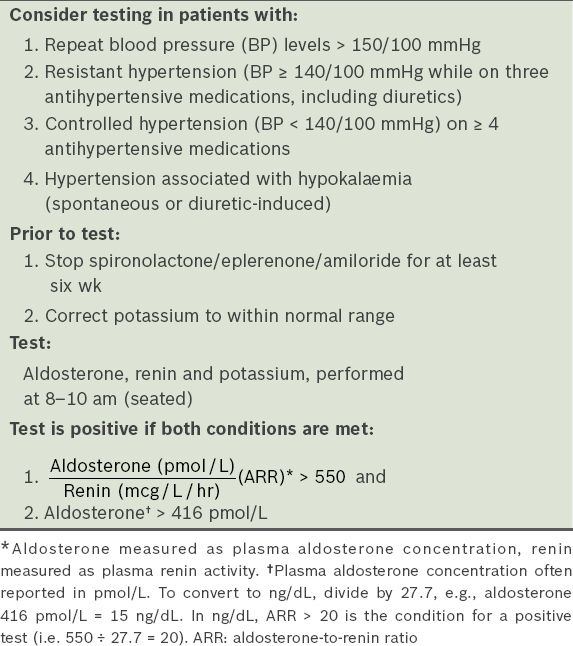
The most important conditions prior to testing are that hypokalaemia is corrected and spironolactone is stopped for at least six weeks. While antihypertensive medications should also be stopped prior to tests (as many affect aldosterone, renin levels and ARR),(16-18) this can be difficult and possibly dangerous.(19) Several medications (e.g. verapamil, hydralazine and prazosin/doxazosin) have minimal effects on ARR and are preferred. If their use is not feasible, we recommend screening patients while keeping them on their current medications,(3-5) and referral to an endocrinologist if the test is positive. The Endocrine Society observed that the current greatest problem is that the screening test is often not performed, leading to an underdiagnosis of this condition.(5)
Renal artery stenosis and renal parenchymal disease
Hypertension due to renal causes can be categorised as resulting from renovascular causes and renal parenchymal disease. Renovascular causes include renal artery stenosis (RAS) due to atherosclerotic disease or fibromuscular dysplasia (FMD), arteritis or extrinsic compression of a renal artery. Renal parenchymal disease includes acute and chronic glomerular diseases, chronic tubulointerstitial disease, polycystic kidney disease, diabetic nephropathy and obstructive uropathy. Based on these aetiologies, the baseline investigations for renovascular causes are serum creatinine test, urinalysis and ultrasonography of the kidneys. Further investigations for renal parenchymal disease are generally based on a nephrologist's assessment.
Clinical situations that alert a physician to RAS are > 30% rise in serum creatinine level after initiation of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin II receptor blocker (ARB), discrepancy in kidney sizes of more than 1.5 cm or recurrent flash pulmonary oedema in a patient with normal left ventricular ejection fraction. The first-line investigation for suspicion of RAS is duplex Doppler ultrasonography of the renal arteries.(20) This is an effective screening test when performed by an experienced vascular radiographer. Magnetic resonance or computed tomographic angiography may be required to confirm the anatomic diagnosis. If there is a high suspicion of RAS requiring intervention, however, the gold standard is renal artery angiography.(21)
Treatment involves correction of modifiable cardiovascular risk factors and control of hypertension. Indications for percutaneous intervention are FMD, short duration of BP elevation prior to diagnosis of RAS and recurrent flash pulmonary oedema. As for atherosclerotic RAS, the first-line treatment is optimal medical therapy to achieve BP targets; if this fails, percutaneous renal revascularisation is indicated.(22)
Obstructive sleep apnoea
OSA is a sleep-related breathing disorder characterised by episodes of complete or partial upper airway obstruction occurring during sleep, resulting in repetitive oxygen desaturation and sleep fragmentation. Typical symptoms associated with OSA include excessive daytime sleepiness, nocturnal gasping or choking events, snoring and unrefreshing sleep. A sleep study (polysomnography) is required for the diagnosis of OSA.
OSA is common, with a recent study placing the estimated prevalence of moderate to severe OSA at 30.5% in Singapore's population.(23) Male gender, obesity and middle age have been identified as associated risk factors.(24) OSA has been strongly associated with hypertension in large cross-sectional and longitudinal studies.(25-27) One study showed that OSA was prevalent in 95% of men and 65% of women with drug-resistant hypertension.(28)
Continuous positive airway pressure (CPAP) is the standard treatment for OSA patients; its primary benefits are the improvement of daytime sleepiness and quality of life.(29) Although CPAP treatment only appears to lower BP by a small margin (~2 mmHg),(30) even a reduction of 1–5 mmHg has been shown to reduce cardiovascular risks significantly.(31) In a recent study, CPAP was able to further decrease the 24-hour mean and diastolic BP in OSA patients with drug-resistant hypertension who were taking an average of 3.8 antihypertensive medications.(32) The magnitude of BP reduction with CPAP is far less than that achieved with antihypertensive medications(33) and these patients should continue to be managed with dietary and lifestyle modifications as well as optimal pharmacotherapy.
Since many patients with OSA remain undiagnosed, a high index of clinical suspicion is needed, particularly in patients with drug-resistant hypertension. The presence of typical symptoms of OSA, such as loud snoring, witnessed apnoea and daytime somnolence, or known risk factors for OSA, should prompt the physician to consider referral to a sleep specialist.
WHEN SHOULD I REFER TO A SPECIALIST?
Referral should be considered when a secondary cause of hypertension is suspected, and the choice of specialist should be based on the likely underlying cause. Other factors that should prompt a referral are young hypertensive patients (< 30 years of age); a positive aldosterone-to-renin ratio with elevated aldosterone level (
After prescribing oral potassium supplements to correct Mr Ali's hypokalaemia, you proceeded to check his aldosterone and renin levels, which were 1,186 pmol/L and 0.15 mcg/L/hr, respectively, with an aldosterone-to-renin ratio of 7,907 (> 550). As this was a positive screening test for primary aldosteronism, you referred him to an endocrinologist. Further tests confirmed the diagnosis of a unilateral adrenal adenoma causing primary aldosteronism. After adrenalectomy, his hypokalaemia resolved, while his hypertension improved to a blood pressure of 124/82 mmHg on only two antihypertensive medications, atenolol and nifedipine.
TAKE HOME MESSAGES
-
Secondary hypertension is a common cause of hypertension in adults, occurring in about 10% of hypertensive patients.
-
Failure to recognise secondary causes can lead to resistant hypertension, cardiovascular complications or complications of the underlying condition.
-
In younger adults (< 30 years of age), renal causes such as glomerulonephritis and coarctation of the aorta should be considered.
-
In older adults, primary aldosteronism, RAS and OSA are common and often underdiagnosed. Screening tests, if available, should be performed to detect these conditions.
-
Diagnosis and treatment of causes of secondary hypertension can lead to good clinical outcomes.


