Abstract
INTRODUCTION
How many orthopods does it take to change a light bulb? One – to refer to the medics for ‘Darkness ?Cause’. Additionally, anaesthetists and surgeons often disagree on the estimated blood loss during surgery and the estimated procedure duration. We designed this study to compare the ability of orthopaedic surgeons and anaesthetists in: (a) estimating fluid volumes; (b) estimating procedure durations; and (c) changing light bulbs.
METHODS
Participants had to either be a specialist in anaesthesia or orthopaedic surgery, or a trainee in that specialty for at least two years. Three different fluid specimens were used for volume estimation (44 mL, 88 mL and 144 mL). Two videos of different lengths (140 seconds and 170 seconds), showing the suturing of a banana skin, were used for procedure duration estimation. To determine the ability at changing light bulbs, the participants had to match eight different light sockets to their respective bulbs.
RESULTS
30 male anaesthetists and trainees and 31 male orthopaedic surgeons and trainees participated in this study. Orthopaedic surgeons underestimated the three fluid volumes by 3.9% and anaesthetists overestimated by 5.1% (p = 0.925). Anaesthetists and orthopaedic surgeons overestimated the duration of the two procedures by 21.2% and 43.1%, respectively (p = 0.006). Anaesthetists had a faster mean time in changing light bulbs (70.1 seconds vs. 74.1 seconds, p = 0.319).
CONCLUSION
In an experimental environment, male orthopaedic surgeons are as good as male anaesthetists in estimating fluid volumes (in commonly seen surgical specimens) and in changing light bulbs. Both groups are poor at estimating procedure durations.
INTRODUCTION
Question: How many orthopaedic surgeons does it take to change a light bulb?
Answer: One; to refer to the medics for ‘Darkness ?Cause’.
Jokes about the intelligence of orthopaedic surgeons are common.(1) In 2011, Subramaniam et al proved that orthopaedic surgeons are as intelligent and twice as strong as anaesthetists,(2) resulting in our anaesthesia colleagues feeling that the comparison was unjust. It is not uncommon for colleagues from these two intimately related specialties to disagree on the estimated blood loss during surgery and estimated procedure duration. Often, we see anaesthetists rolling their eyes upon hearing the orthopaedic surgeon’s underestimation of blood loss during surgery and attempts at over-listing cases in the elective theatre (which affects the anaesthetists’ ability to leave the hospital at 5 pm).
Based on the Surgical Safety Checklist published by the World Health Organization, the ability of the surgeon to accurately estimate the amount of blood loss before the start of surgery is important.(3) Good estimation of blood loss can allow rapid and adequate fluid and blood product resuscitation of the surgical patient.(4) Good estimation of the time taken to complete a surgery is also important as it allows anaesthetists to better titrate anaesthetic drugs and enables a smoother overall workflow for the operating list. In an attempt to settle the ‘dispute’ between orthopaedic surgeons and anaesthetists, the present study was designed to indirectly assess the ability of orthopaedic surgeons and anaesthetists to estimate fluid volumes, estimate procedure duration and change light bulbs.
METHODS
This study was a prospective, multicentre, comparative study. Participants were recruited from three hospitals over a one-month period. To be eligible for inclusion in this study, participants had to be either: (a) a specialist in anaesthesia or orthopaedic surgery; or (b) a trainee in either of the two aforementioned specialties, with a minimum of two years’ experience in that specialty. The three hospitals involved were visited on random days and the tests were conducted in the operating room pantry or common areas. All orthopaedic surgeons and anaesthetists who passed by these areas on those days were invited to participate. Only male participants were included in this study, due to the lack of eligible female participants.
As an indirect method of testing the participants’ ability to estimate surgical fluid loss, we prepared three different watertight bags with commonly used surgical materials soaked with random volumes of fluid – (a) two pieces of surgical gauze swabs (4 inches × 4 inches) soaked with 44 mL of pink chlorhexidine; (b) one piece of surgical sponge towel (12 inches × 12 inches) soaked with 144 mL of pink chlorhexidine; and (c) a catheter collection bag filled with 288 mL of iodine-tinged saline (
Fig. 1
Photographs show (a) Specimen 1 with 44 mL of fluid; (b) Specimen 2 with 144 mL of fluid; and (c) Specimen 3 with 288 mL of fluid.

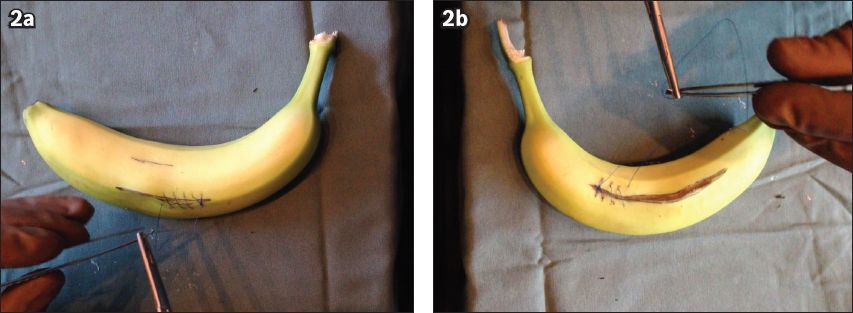
To test the participants’ ability to estimate procedure duration, we prepared two videos of different durations (
Fig. 2
Still capture of (a) Video 1 shows an incised banana being sutured; and (b) Video 2 shows an incised banana, with a visibly longer incision, being sutured.
To measure the participants’ ability to change light bulbs, they were given a stopwatch and a plastic bowl on a wooden board with eight different light sockets attached to it (
Fig. 3
Photographs show (a) light bulb test setup; (b) light sockets; and (c) light bulbs.

Data was collected on a Microsoft Excel 2010 spreadsheet (Microsoft, Redmond, WA, USA) and analysed with IBM Statistical Package for the Social Sciences version 20 (IBM Corp, Armonk, NY, USA). Based on our hypothesis that it takes as many orthopaedic surgeons as anaesthetists to change a light bulb, the sample size was calculated on a type 1 error of 0.05 and a type 2 error of 0.2. An a priori analysis performed on the first 20 participants resulted in a mean ± standard deviation of 75 ± 18 seconds. To detect a 15% difference in time to change light bulbs, we needed 31 participants in each group. Non-parametric data was analysed using the Mann-Whitney U test. To calculate the mean percentage error for the groups, we first calculated the average percentage error (across all three volumes and both timings) for each participant. From this result, the mean percentage error for the group was obtained.
RESULTS
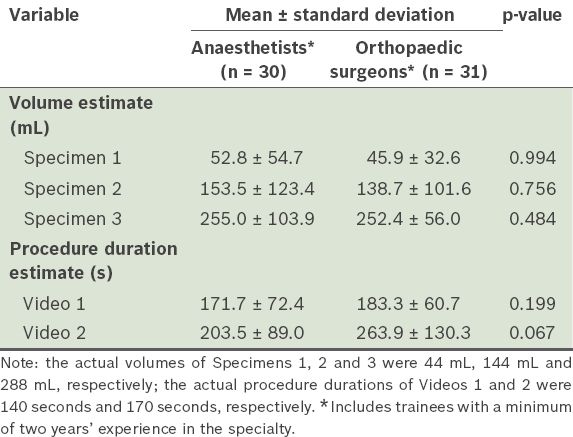
A total of 30 male anaesthetists and trainees (mean age 43 years, mean 15 years of experience) and 31 male orthopaedic surgeons and trainees (mean age 38 years, mean 10 years of experience) were recruited over the one-month study period (
Table I
Demographics and overall results of the participants (n = 61).
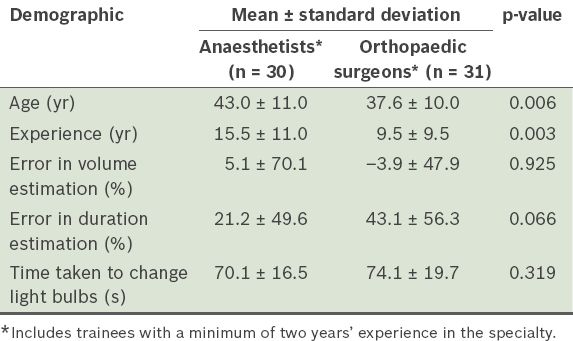
Orthopaedic surgeons underestimated the three volumes by 3.9%, while anaesthetists overestimated the volumes by 5.1% (
Table II
Volume and procedure duration estimates of the participants (n = 61).
DISCUSSION
The aim of the present study was to prove that there was no significant difference between orthopaedic surgeons and anaesthetists in their ability to estimate volumes, estimate procedure duration and complete the common task of changing bulbs. Accurate estimations of fluid losses during surgery and surgical procedure duration would allow optimal patient care and efficient utilisation of operating theatre resources. Furthermore, as both surgeons and anaesthetists have to review their postoperative patients, plan for the next day’s operating schedule and perform non-clinical duties after completing their operating lists, the ability to complete the operating list on time would allow both groups to attend to other work commitments in a timely manner.
Volume estimation in the present study was surprisingly accurate in both groups, with a less than 5% error in estimation. Actual intraoperative fluid and blood loss is determined by measuring the amount of fluid in the suction canister and urine catheter, and by weighing surgical swabs.(5) It is known that visual estimation is prone to error (overestimating at low volumes and underestimating at high volumes).(6) In the case of paediatric spinal surgeries, Mooney et al concluded that orthopaedic surgeons had higher estimates for blood loss than anaesthetists.(7)
In the present study, both the orthopaedic surgeons and the anaesthetists were unable to accurately estimate procedure durations. In fact, the orthopaedic surgeons overestimated the procedure duration by 43.1%, while the anaesthetists overestimated by 21.2%. This result is unexpected, as it is popular belief that surgeons underestimate their surgical procedure duration and overestimate their operative ability. Although a study has concluded that surgeons provide significantly better estimates than computerised scheduling systems, there is still no consensus on whether the use of surgeons’ estimates or historical surgical procedure durations are better in reducing the number of procedures that finish late.(8,9) A very plausible explanation for our finding of gross overestimation of procedure duration (i.e. banana suturing) by both the orthopaedic surgeons and the anaesthetists is that an observer of a procedure tends to feel that the procedure is proceeding very slowly (be it a regional anaesthetic block or suturing of a wound). Future studies could be modified to improve on this element, by asking participants to estimate the time taken for them to perform a suturing task and actually perform the task subsequently.
In terms of the time taken to change the light bulbs, the result was largely similar between the two groups, proving that orthopaedic surgeons and anaesthetists were similarly capable at this task. A separate analysis performed, with age and experience as the denominator, did not reveal that younger persons were worse at changing light bulbs, contrary to our senior author’s hypothesis. A potential source of error in the present study was the mismatch between the age and experience of the participants in the two groups. However, age and experience have not been proven to be associated with the ability to perform the three tasks evaluated in this study.
In a literature search that we conducted (in an attempt to account for any differences that may have occurred between the two groups), we found that orthopaedic surgeons have been portrayed as more aggressive and gorilla-like; they were also shown to enjoy golf as a sport.(10-12) On the other hand, previous studies on the characteristics of anaesthetists reveal that they are more cooperative and harm-avoidant, and less novelty-seeking and reward-dependent.(13,14) One correspondence article unveiled why anaesthetists have a special affinity for crossword puzzles.(15)
The strengths of the study include a prospective multicentre design and an adequate sample size. Also, the tests conducted were accurately and consistently replicated among all the participants. However, the present study was not without limitations. The testing material is novel and has not been proven to accurately correlate with the performance of the specialists in an actual clinical environment. Our light bulb setup also does not fully replicate the real-world process of changing light bulbs. The estimations of volume loss and procedure time could have been performed in an actual clinical environment to reflect the real-life scenario more accurately. We also had to exclude female participants so that any confounders due to gender differences could be eliminated (neither were there sufficient women in the sample for a meaningful analysis). The random nature of participant invitation meant that not all potentially eligible participants from all three institutions were included in the study. The difference in the mean age of the two groups may also have been a potential confounder (a group of younger orthopaedic surgeons were compared with a group of older anaesthetists). One possible explanation for this age difference is that anaesthetists have a longer career lifespan, and being less reward-dependent, there may have been more likely to continue working in one of the three public hospitals that were involved in this study.
To conclude, in a testing environment, orthopaedic surgeons are as good as anaesthetists in: (a) estimating fluid volumes in commonly seen surgical specimens; (b) estimating the time taken to complete a commonly seen surgical procedure; and (c) changing light bulbs. An orthopaedic surgeon’s estimate of fluid loss during surgery should not be discounted by their anaesthetist colleagues. Both groups of specialists are poor at estimating procedure duration. The findings of the present study may form the basis for future clinical studies, which may have results that can be extrapolated to an actual clinical environment. And to answer the question of how many orthopaedic surgeons it takes to change a light bulb, the answer is that it takes as many orthopaedic surgeons as it does anaesthetists to change a light bulb (although they may be occupied with golf or crossword puzzles).


