Abstract
INTRODUCTION
As the population ages, the prevalence of hypertension also increases. Although primary care is usually the patient’s first point of contact for healthcare, little is known about the management of hypertension among elderly patients at the primary care level. This study aimed to determine the antihypertensive prescription trend for elderly patients, the predictors of antihypertensive use and any inappropriate prescribing practices in both public and private primary care settings.
METHODS
Data on patient demographics, diagnosis, prescription pattern, payment mode and follow-up was extracted from a cross-sectional study involving 122 public primary care clinics and 652 private primary care clinics in Malaysia. Encounters with hypertensive patients aged ≥ 60 years were included.
RESULTS
A total of 1,017 antihypertensive medications were prescribed – calcium channel blockers (27.1%), beta blockers (25.5%), diuretics (23.3%), angiotensin-converting enzyme inhibitors (14.9%) and angiotensin receptor blockers (6.3%). Out of the 614 patient encounters, 53.1% of the patients were prescribed monotherapy, 31.6% were prescribed dual therapy, 12.2% triple therapy, 2.8% quadruple therapy and 0.3% quintuple therapy. Type of primary care clinic and payment mode were significant predictors for the prescription of combination therapy and fixed-dose combination therapy, respectively. Four types of inappropriate prescriptions were identified.
CONCLUSION
Calcium channel blockers were the most common antihypertensive drug prescribed and more than half of the elderly patients were on monotherapy. Antihypertensive drug prescription was found to be associated with the type of primary care clinic and the payment mode, suggesting that prescription is influenced by the cost of the drug.
INTRODUCTION
The prevalence of hypertension increases with age.(1) Therefore, the burden of hypertension is expected to rise with the world’s rapidly ageing population. In the United Kingdom, more than 50% of persons aged > 60 years have hypertension.(1) In Malaysia, the proportion of people with hypertension was reported to be 74.1% for persons aged 65–69 years, 68.7% for persons aged 60–64 years, 44.0% for persons aged 45–49 years, and 22.2% for persons aged 30–34 years.(2)
Five major classes of drugs are used in the treatment of hypertension, namely angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta blockers (BBs), calcium channel blockers (CCBs) and diuretics (DUs). These drugs have been shown to reduce cardiovascular events in elderly patients and are recommended for use in various treatment guidelines.(1,3,4) Other less commonly used drugs include centrally acting drugs (CADs) and alpha blockers (ABs). ABs are sometimes used in the presence of certain comorbidities such as benign prostatic hyperplasia.(3)
The treatment goals for hypertension among elderly patients are similar to those for hypertension among younger patients: to lower the patient’s blood pressure (BP) and to prevent major cardiovascular events that are attributable to hypertension.(1,4) In general, drug treatment in elderly patients aims to use the least number of drugs to control BP, and the reduction in BP should be gradual so as to minimise the risk of ischaemic events (especially in patients with postural hypotension).(3,4)
In elderly patients, the choice of antihypertensives should be individually tailored depending on the individual’s cardiovascular risk, presence of target organ damage, comorbidities and potential adverse drug effects (especially for postural hypotension). It is important to note that elderly patients are more prone to adverse drug effects than younger patients.(5)
For patients on multiple drugs, fixed-dose combination (FDC), which is the combination of two antihypertensive drugs in a single tablet, has been shown to improve compliance and cause reductions in BP similar to its corresponding free-drug components.(6) However, the cost of FDC therapy is high and it is still inconclusive whether its clinical benefits merit the high costs.(7)
While many factors affect the use of antihypertensive drugs in elderly patients, to date, there has been no study conducted in Malaysia to elucidate how antihypertensive drugs are prescribed for the ageing population in the primary care setting. Malaysia has a two-tier healthcare system, with its primary care service provided by both publicly funded health centres and privately owned general practices. According to the Third Health and Morbidity Survey 2006,(8) at least 60% of the Malaysian population aged ≥ 60 years utilised primary care facilities for recent illnesses. The rate of visits for hypertension in private general practices was found to be 1.69 per 100 patient encounters;(9) this value is expected to be higher in public health centres due to the heavy subsidy for healthcare costs that are available in those centres.(10) Previous studies have found that there is a lack of evidence-based practice in the prescription of drugs for hypertension among primary care doctors in Malaysia.(10,11) Therefore, the aim of the present study was to: (a) determine the antihypertensive drug prescription pattern for elderly patients; (b) investigate if there are differences in the prescription patterns for patients attending different types of primary care clinics (i.e. public and private); and (c) determine the predictors of the use of combination therapy and FDC therapy. The study also aimed to identify inappropriate prescribing patterns. Findings from the study would help generate insights on the current practices in hypertension management for elderly patients in both the public and private primary care settings.
METHODS
The present study used data from the National Medical Care Survey (NMCS),(12) a large cross-sectional study that was conducted between 1 December 2009 and 30 April 2010 among 150 public primary care clinics and 1,495 private primary care clinics in Malaysia. The clinics were selected using a mixed mode sampling technique (stratified random sampling by states for public health clinics and convenience sampling for private clinics) due to the heterogeneity between the two types of primary care clinics. Participation of clinics in the NMCS was voluntary. Each participating clinic was randomly assigned a date for data collection. Data regarding patient encounters was collected using self-administered standard data collection forms, which were completed by the doctors. Data collected included patient demographics, reason(s) for visit, payment mode, visit disposition and drugs prescribed. A notice about the study was displayed in participating clinics on the day of the survey. Patients could decline having their data recorded if they wished to be excluded from the survey.
Out of the clinics sampled, 122 (81.3%) public clinics and 652 (43.6%) private clinics responded with 4,173 and 17,695 patient encounters, respectively. The patients’ reasons for the clinic visits were coded using International Classification of Primary Care Second Edition (ICPC-2) codes,(13) while the drugs prescribed to the patients were coded using the Anatomical Therapeutic Chemical classification system.(14,15) The NMCS was approved by the Malaysian Ministry of Health Research and Ethics Committee (MRG grant no. NMRR-09-842-4718). Further details on the methodology of the survey are described in the NMCS report.(12)
All patient encounters that involved elderly patients citing hypertension as a reason for the clinic visit were included in the present study. Patients aged ≥ 60 years were considered elderly, in accordance with the definition found in the Malaysian National Policy for the Elderly.(16) Patient encounters that had missing or incomplete drug prescription details and/or no antihypertensive drugs prescribed were excluded. The antihypertensive drugs prescribed were categorised into the following groups: ACE inhibitors, ARBs, BBs, CCBs, DUs, CADs and ABs. Patients were assumed to be taking only the drugs prescribed during the clinic visit for their hypertension. The type of therapy prescribed was determined based on the number of antihypertensive drugs prescribed to the patient during the patient encounter – if a single antihypertensive drug was prescribed, it would be categorised as monotherapy; if two drugs were prescribed, it would be categorised as dual therapy, and so on. An FDC therapy was also considered dual therapy. Dual, triple, quadruple and quintuple therapies were collectively known as combination therapy. Free combination therapy was defined as the prescription of two or more drugs during the same encounter without the use of FDCs.
Data management and statistical analysis were done using Microsoft Office Excel 2007 (Microsoft Corp, Redmond, WA, USA) and IBM Statistical Package for the Social Sciences software version 20.0 (IBM Corp, Armonk, NY, USA), respectively. Descriptive statistics was used to describe the antihypertensive drug prescription pattern. Chi-square test was used to compare data between categories. Two multiple logistic regression analyses (forward selection) were performed to determine the predictors of combination therapy prescription and FDC therapy prescription. In both regressions, either payment mode (i.e. government subsidy, out-of-pocket or private third party) or type of primary care clinic (i.e. public or private) was included as an independent variable. This was because all public clinics were funded by the government, while all private clinic prescriptions were paid either by the patients themselves (i.e. out-of-pocket) or by private third party payers. If both variables were included in the same regression, it would result in multicollinearity. A p-value < 0.05 (two-tailed) was considered statistically significant.
RESULTS
In NMCS, 2,701 of the 21,868 patient encounters (12.4%) involved elderly patients. Among those elderly patient encounters, 709 (26.2%) were encounters that had hypertension as a reason for the visit. After excluding 51 encounters that had missing or incomplete drug details and 44 encounters in which no antihypertensive drugs were prescribed, the final sample analysed consisted of 614 patient encounters (44.6% from public clinics, 55.4% from private clinics). The mean age of the elderly patients was 68.6 ± 6.5 (range 60–93) years.
A total of 1,017 antihypertensive drugs were prescribed during the 614 patient encounters. The mean number of drugs prescribed per encounter was 1.80 ± 0.87 in public clinics and 1.54 ± 0.76 in private clinics.
Table I
Antihypertensive drugs prescribed in elderly patients (n = 1,017).
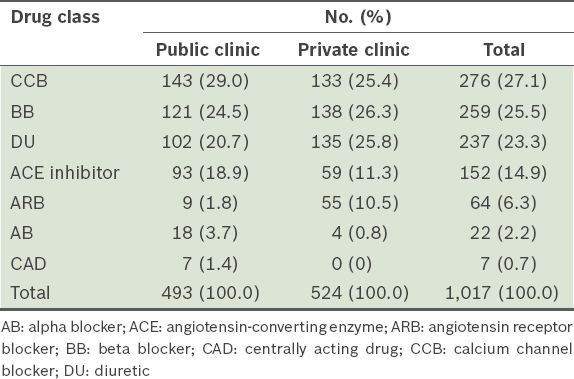
Table II
Antihypertensive drugs prescribed for elderly patients on monotherapy (n = 326).
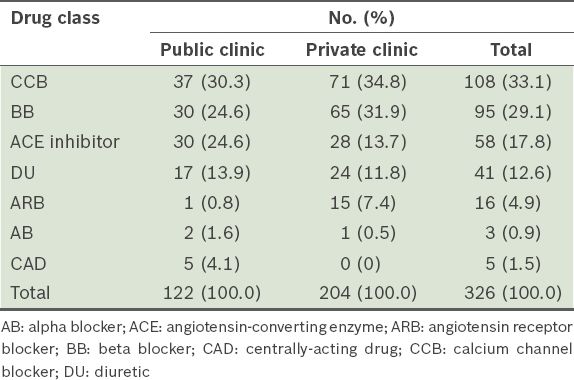
Among patients on CCB monotherapy, more than half (53.7%) were prescribed amlodipine; the remaining were prescribed nifedipine (40.7%) or felodipine (5.6%). Atenolol was the most frequently prescribed BB; it comprised nearly 75% of all monotherapy BB prescriptions. The most frequently prescribed ACE inhibitor among those on monotherapy was perindopril (50.0%), followed by enalapril (31.0%). Nearly all DU prescriptions for monotherapy were hydrochlorothiazide (46.3%) or indapamide (41.5%). Telmisartan (43.8%) was the most commonly used ARB in monotherapy. The three most preferred antihypertensive drugs for monotherapy in public clinics were nifedipine (21.3%), perindopril (18.9%) and atenolol (15.6%), while those for monotherapy in private clinics were atenolol (25.5%), amlodipine (24.0%) and nifedipine (8.8%).
Dual therapy was prescribed in 194 patient encounters. Among them, there were 18 different drug combinations prescribed. In both public and private clinics, the most common combination was CCB + BB (approximately 20%). Other combinations used were BB + DU (17.0%), ACE inhibitor + CCB (11.9%), CCB + DU (10.3%) and ARB + DU (9.2%). There were only 31 prescriptions for FDC dual therapy, nearly all of which (96.9%) were prescribed in private clinics. Most of the dual therapies in the public clinics (98.9%) were free combination.
Triple therapy was prescribed in 75 patient encounters; seven unique combinations were seen in the public clinics (40 patient encounters), while 11 unique combinations were seen in the private clinics (35 patient encounters). All triple therapy combinations included one CCB or at least one DU. In cases where two DUs were prescribed, nearly all DU + DU combinations (88.9%) were amiloride and hydrochlorothiazide (i.e. co-amilozide). A third of the triple therapy prescriptions made in public clinics were combinations of BB + CCB + DU.
About 3.1% of the study population was given 4–5 antihypertensive drugs. One quintuple therapy was observed in a public clinic and one in a private clinic. The five-drug combinations were AB + ACE inhibitor + BB + BB + CCB (public clinic) and ARB + BB + CCB + DU + DU (private clinic).
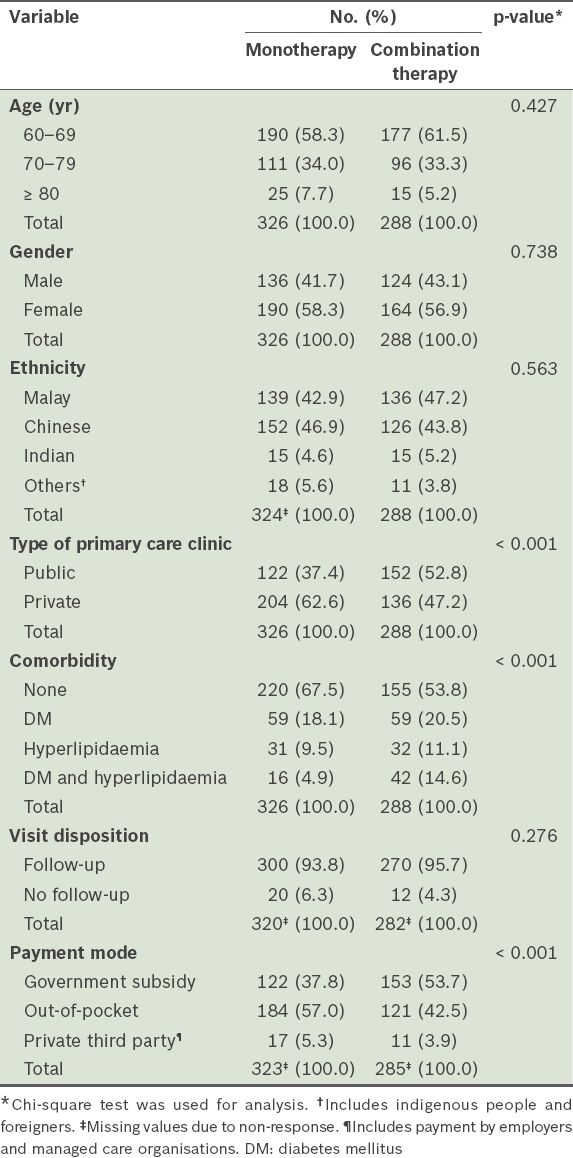
Of the 614 patient encounters, 53.1% of the patients were on monotherapy, 31.6% were on dual therapy, 12.2% were on triple therapy, 2.8% were on quadruple therapy and 0.3% on quintuple therapy. Significant associations were found between type of therapy (monotherapy or combined therapy) and type of primary care clinic (public or private), presence of comorbidities (diabetes mellitus and/or hyperlipidaemia) and payment mode (
Table III
Characteristics of elderly patients with hypertension (n = 614), according to the type of therapy prescribed.
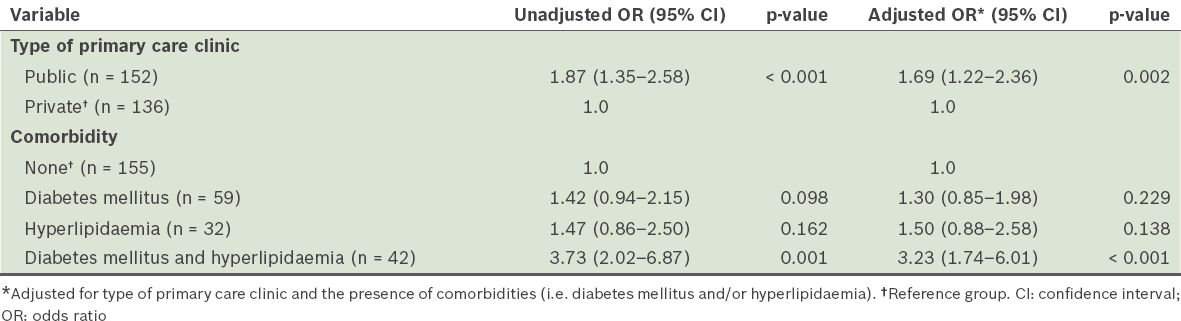
The results of the logistic regression analysis are shown in
Table IV
Results of the logistic regression analysis of elderly hypertensive patients who were prescribed combination therapy (n = 288).
FDC therapy was prescribed in 70 of the 614 patient encounters (11.4%). Significant associations were found between FDC therapy prescription and type of primary care clinic, payment mode and type of therapy (
Table V
Characteristics of elderly hypertensive patients who were prescribed fixed-dose combination (FDC) therapy and those who were not (n = 288).
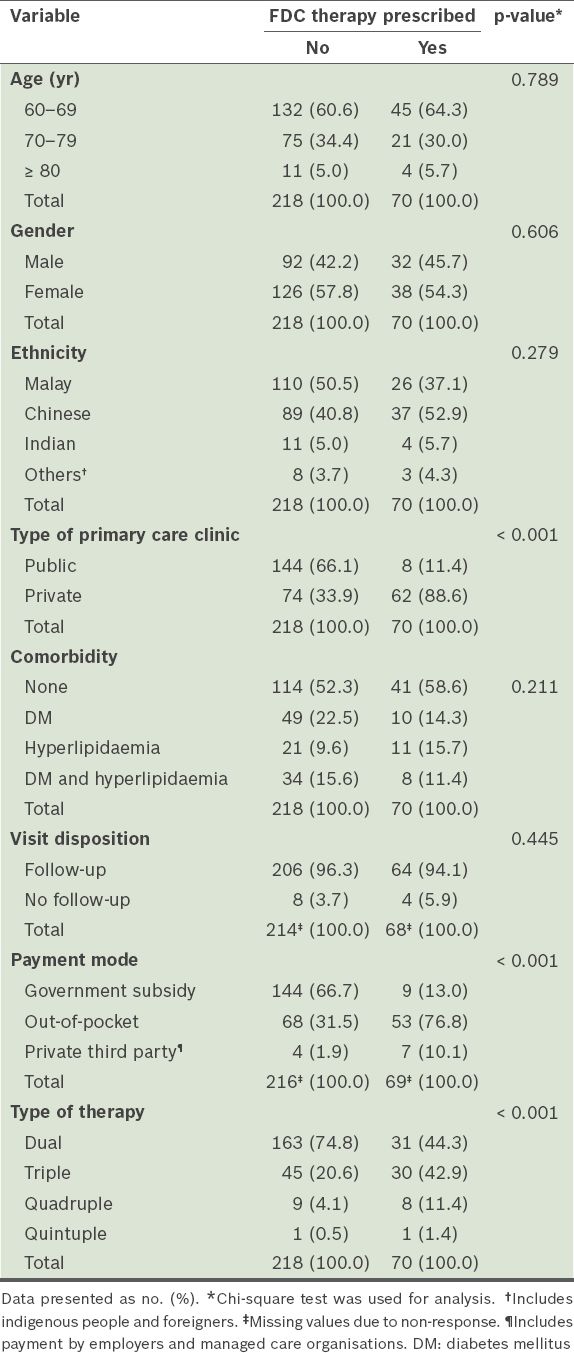
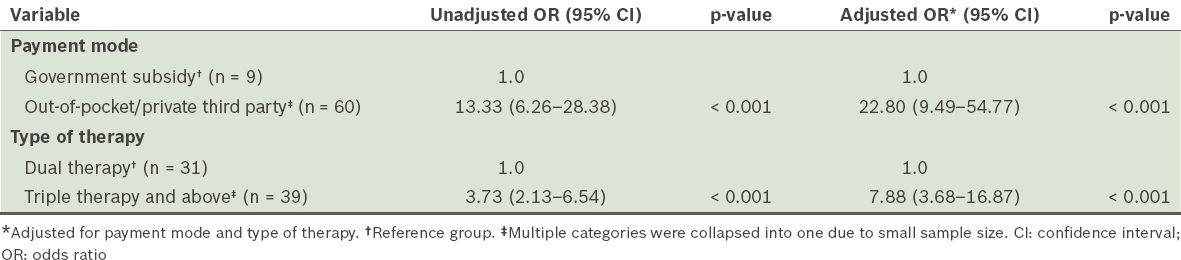
Table VI
Results of the logistic regression analysis of elderly hypertensive patients who were prescribed fixed-dose combination drugs.
Four types of inappropriate prescriptions were identified. First, there was a prevalent use of short-acting nifedipine for hypertension. Only 13.2% (16/121) of all nifedipine prescriptions were long-acting preparations. The second type of inappropriate practice was the prescription of prazosin or methyldopa as monotherapy; this, however, only affected a minority (2.5%) of the patients (
DISCUSSION
The present study has four important findings: (a) the antihypertensive drug prescription pattern for elderly patients differed between public and private primary care clinics; (b) predictors of the use of combination therapy were the type of primary care clinic and the presence of comorbidities (diabetes mellitus and hyperlipidaemia); (c) predictors of the use of FDC were the payment mode and the type of therapy (dual therapy vs. triple therapy and above); (d) four types of inappropriate prescribing patterns were identified – prevalent use of short-acting nifedipine, use of AB or CAD as monotherapy, inappropriate dual therapies (e.g. combinations of BB + DU and DU + DU) and the use of two different drugs from the same class in quintuple therapies.
Overall, the most commonly used antihypertensive drug in the present study was CCBs. While BBs were the most commonly prescribed antihypertensive medication in the private clinics, they were only the second most commonly prescribed antihypertensive medication in public clinics. This difference could be attributed to the different structures of the public and private primary care clinics, as well as the different incentives they receive. For instance, the private primary care clinics in the present study were made up of general practitioners, the majority of whom were aged > 45 years (61%)(17) and in solo practice (78%).(18) Therefore, the prevalence of dated practices, such as the prescription of BBs for elderly patients with hypertension, in the private clinics (
Patients visiting public clinics and those with comorbidities of diabetes mellitus and hyperlipidaemia were more likely to be prescribed combination therapy. Patients attending public clinics in Malaysia only need to pay a nominal fee of RM 1 (USD 0.30) for each consultation, including the medication prescribed during that consultation. As patients who attend public clinics tend to have a higher prevalence of comorbidities,(20) a higher number of them would have received combination therapy. However, the budget cap in public clinics would have limited the number of FDC therapies prescribed. Prescriptions for FDC therapy were found to be more frequent among patients who: (a) were either self-funded (i.e. paid out-of-pocket) or funded via private third party insurance; and (b) received triple or more therapies. In the present study, the private clinics were shown to have a higher prescription rate for ARBs than ACE inhibitors, even though the former is more expensive and there is a lack of evidence supporting its superiority over ACE inhibitors.(21) A possible reason for this observation is that ARBs, as compared with ACE inhibitors, have a lower incidence of persistent dry cough.(4) This could help improve patient adherence to the medication, and thus, leads to less ‘doctor shopping’.
Although 70% of the elderly population could have hypertension,(2) the elderly hypertensive patients in the present study made up only slightly over a quarter of all elderly patients seeking treatment in primary care clinics. This could be, in part, due to underdiagnosis. The rate of undiagnosed hypertension among Malaysians aged ≥ 60 years was reported to be nearly 30%.(2)
The mean number of antihypertensive drugs prescribed per encounter in the present study was lower than that observed in several major clinical trials, where at least two antihypertensive drugs were needed to achieve target BP.(22) It is uncertain if this could be attributed to undertreatment, as the data source did not contain any information regarding the patient’s clinical parameters and acceptability of the drugs. The data source also did not have information on whether the patient had any previous intolerance to other antihypertensive drugs.
With regard to the inappropriate practices identified in the present study, the prescription of short-acting nifedipine for hypertension was also observed in an earlier study.(11) Short-acting nifedipine is not recommended for use in elderly patients due to its association with increased cardiac events.(3,4) Its high prescription rate in the present study was likely due to it having the lowest recommended wholesale and retail price in both public(23) and private clinics,(24,25) as listed on the National Essential Drug List (NEDL). Excluding amlodipine, the top three preferred antihypertensive monotherapies in both the public and private clinics are also listed in the NEDL. Practice guidelines recommend against the use of prazosin and methyldopa as monotherapy.(1,3-5) Meanwhile, BB + DU and co-amilozide dual combinations might be inappropriate for elderly patients, as these combinations are linked to a higher risk of new-onset diabetes mellitus(1,4) and a higher incidence of diabetes mellitus and secondary events,(26) respectively, when compared with long-acting nifedipine.
The present study demonstrated that differences in the type of clinic (public vs. private) and payment mode could influence the prescription pattern of antihypertensive drugs for elderly patients. Policymakers should pay attention to such differences, as they are likely to lead to different outcomes between patients who visit public clinics and those who visit private clinics. Other than that, interventions are required to address the systematic prescribing errors in both types of clinics. Interventions could be in the form of: (a) an update in the NEDL and/or clinical practice guidelines; (b) educational intervention; and/or (c) safety-netting of prescriptions by a pharmacist. Pharmacists are currently mostly available in public clinics located in urban areas of Malaysia. Further studies can be carried out to elucidate the reasons behind the high prevalence of BB prescriptions for elderly patients with hypertension. Studies can also be conducted to compare the outcomes of patients visiting different types of clinics (public vs. private) for hypertensive care, particularly in terms of FDC therapy utilisation.
The present cross-sectional study was not without limitations. It was limited by the small number of patient encounters, reports of patient encounters by doctors and convenience sampling of private clinics. Convenience sampling was done due to the lack of a sampling frame for private clinics. However, it was the best possible method that could be employed at the time of the study. The prescription patterns of antihypertensive drugs could also be affected by other factors, including physicians’ knowledge and background, pharmaceutical companies’ influence, physicians’ satisfaction toward the use of the drug and physicians’ prescription habits acquired over time.(27) However, as the present study was observational in nature, those factors were not examined. Future studies could be done to examine the influence of those factors. The exclusion of 13.4% of patient encounters in the present study due to missing/incomplete details or no antihypertensive drugs prescribed could have also been a potential source of bias.
To conclude, we found that more than half (53.1%) of the elderly patients in the Malaysian primary care setting were prescribed monotherapy for hypertension. The maximum number of antihypertensive drugs prescribed per patient was five and the most preferred therapeutic class of antihypertensive drugs was CCBs (contributed mainly by prescriptions made in the public clinics), followed by BBs, DUs, ACE inhibitors and ARBs. The type of clinic (public vs. private) and the payment mode were found to be significant predictors of the use of combination therapy and FDC therapy, respectively, indicating that prescription patterns may be influenced by medication cost. Four types of inappropriate prescriptions were identified in the present study – the use of short-acting nifedipine, the use of ABs and CADs as monotherapy, the use of dual therapies that are associated with adverse effects among elderly patients and the practice of polypharmacy. Further education is needed to improve the management of hypertension in elderly patients.
ACKNOWLEDGEMENTS
We would like to thank the Director General of the Ministry of Health, Malaysia, for his permission to publish this manuscript. We would also like to express our gratitude to Mr Adam Bujang for his advice on the statistical analysis used and the NMCS project team members for their contribution to the present study. The design, methodology, data collection, analysis and data interpretation, as well as the writing and submission of the present manuscript, were fully independent of the funding agencies. Part of this manuscript was presented orally at the 1st Asia Pacific Clinical Epidemiology & Evidence Based Medicine (APCEEBM) Conference in Kuala Lumpur, Malaysia, on 8 July 2012.


