Abstract
Abstract A 53-year-old man presented with acute cervical myelopathy following a fall. Cervical radiography and computed tomography showed ossification of the posterior longitudinal ligament (OPLL) from C2 to C6 level, with severe cervical canal stenosis and cord compression. Magnetic resonance imaging further showed increased T2-weighted signal in the spinal cord at the level of greatest central spinal canal stenosis. OPLL is a significant cause of myelopathy in Asian populations and is found in up to 25% of patients presenting with cervical compression myelopathy. The clinical presentation, radiological evaluation and management of OPLL are discussed.
CLINICAL PRESENTATION
A 53-year-old man presented with acute weakness of all four limbs (more on the right side) after an assault, during which he fell on his right side. He reported no urinary problems, but had not had any bowel movement for the past five days.
On examination, the patient had bilateral hypoaesthesia from the C5 to T1 level. Muscle strength in both upper limbs was decreased, with the right side affected more than the left. Muscle strength was also markedly reduced (1/5) in the right lower limb but full (5/5) in the left lower limb. Reflexes were graded 3+ in both upper limbs and the right lower limb, and 2+ in the left lower limb. Babinski reflex was negative. Abdominal examination was significant for a palpable, distended bladder and urinary catheterisation yielded 1,100 mL of urine. Sphincter tone was normal.
A cervical spine radiograph (
Fig. 1
Lateral radiograph of the cervical spine.

Fig. 2
Sagittal (a) T2-W and (b) T1-W MR images of the cervical spine.
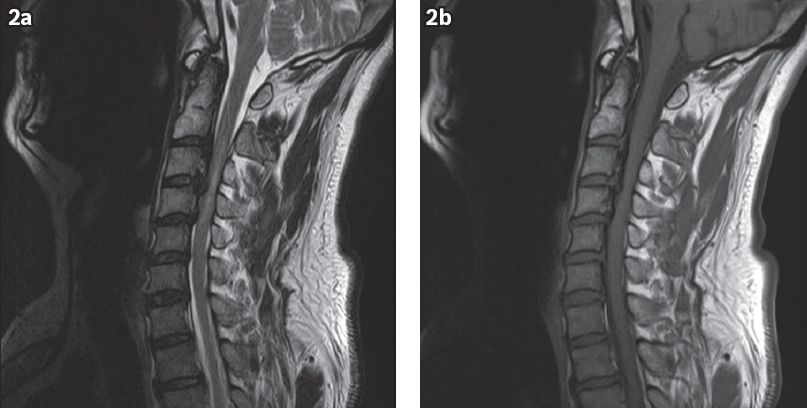
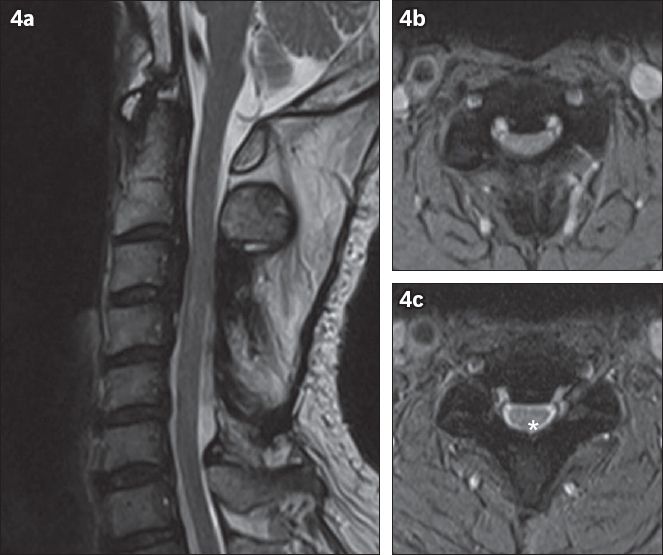
Fig. 3
(a) Sagittal and (b) selected axial CT images of the cervical spine.
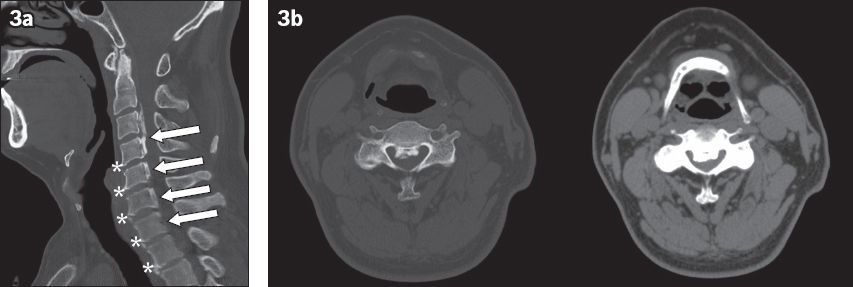
IMAGE INTERPRETATION
The lateral cervical spine radiograph (
MR image of the cervical spine (
CT image of the cervical spine shows a mixed-type OPLL, with continuous ossification extending from the inferior border of the C2 vertebral body to the inferior border of the C4 vertebral body, and segmental ossification at C5 and C6 levels (arrows indicating C2 to C6,
DIAGNOSIS
Cervical OPLL with cord compression.
CLINICAL COURSE
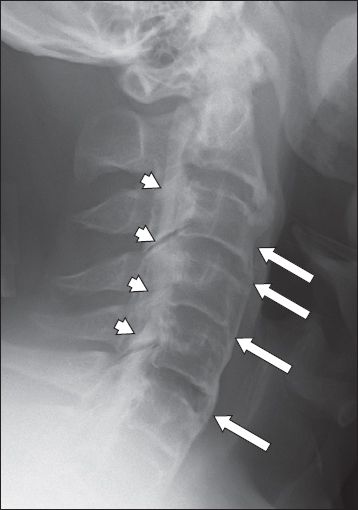
The patient underwent a C3 to C6 double trap door laminoplasty on Day 2 of admission. Postoperative recovery was uneventful, with marked improvement in muscle strength of his right lower limb from 1/5 to 4/5 and mild improvement in bilateral upper limb muscle strength. Hypoaesthesia was still present from C5 to T1 level with minimal improvement. Neurogenic bowel and bladder symptoms resolved postoperatively and he was able to micturate with minimal post-void residual urine. Repeat MR imaging three months post-surgery showed improvement in spinal canal stenosis and reduction in intramedullary T2-weighted signal (
Fig. 4
(a) Sagittal T2-W postoperative MR image shows improvement in spinal canal stenosis and reduction in intramedullary T2-W signal. (b) Preoperative and (c) postoperative axial T2-W MR images at level C3/4 show improvement in central spinal canal stenosis after laminoplasty. Note the reappearance of cerebrospinal fluid posterior to the spinal cord post-surgery (* in c).
DISCUSSION
OPLL is the pathological replacement of the posterior longitudinal ligament (PLL) in the spine with lamellar bone. It predominantly affects men, the elderly and Asians, and is found in up to 25% of patients presenting with cervical compression myelopathy.(1)
First described in Japanese patients, OPLL is a significant cause of myelopathy in Asian populations, particularly East Asians. It has an incidence of 2%–4% in Japan, Korea and Taiwan,(2) compared to an incidence of 0.12% in North America.(3) In Singapore, the incidence of OPLL was 4% in a 1991 study of patients presenting with neck pain at a private hospital.(4)
The pathogenesis of the disease remains poorly understood, with multiple mechanisms involved, including genetics, environment, hormonal factors and lifestyle factors. It may occur in isolation or in association with other musculoskeletal diseases, such as diffuse idiopathic skeletal hyperostosis (
Fig. 5
Lateral cervical spine radiograph of a patient with diffuse idiopathic skeletal hyperostosis shows ossification of the anterior longitudinal ligament (arrows) in addition to marked ossification of the posterior longitudinal ligament (arrowheads). Note the preservation of the height of the intervertebral disc spaces.
OPLL is twice as common in men as in women and tends to present in patients in their 40s or 50s. Most patients with OPLL are asymptomatic, but those with significant stenosis may present with neurological symptoms such as pain, radiculopathy, myelopathy, and bladder and bowel symptoms. While the onset is typically gradual and progressive, up to 15% of symptomatic patients will present acutely following even minor trauma (e.g. a fall), as was seen in our patient.
A full neurological physical examination should be performed to assess for myelopathy. Sensation, muscle strength, and reflexes of both the upper and lower extremities should be tested to assess the level of involvement. Unsteady gait should also be assessed with heel- and toe-walking as well as tandem walking.
The first step in radiologic evaluation of cord compression syndrome and OPLL is plain radiography, visualised on lateral views as dense ossification immediately posterior to the vertebral bodies (
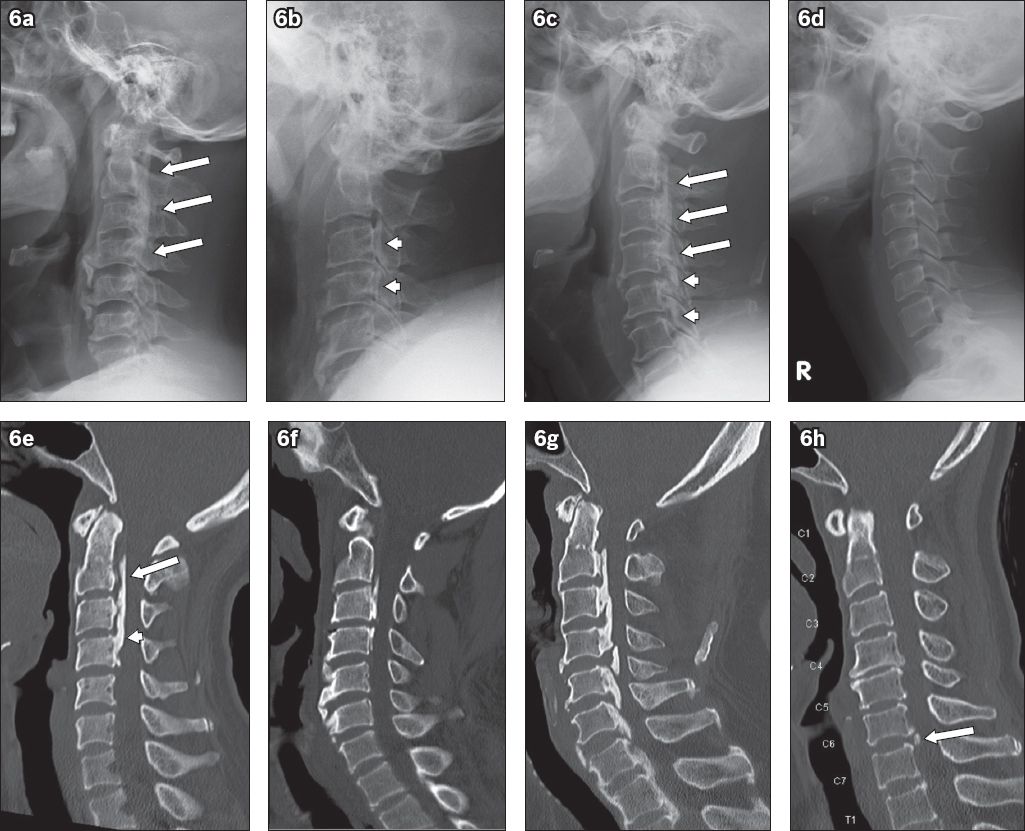
Fig. 6
Top row: classification of ossification of the posterior longitudinal ligament (OPLL) subtypes on lateral cervical radiograph: (a) continuous (arrows show extent of the continuous type); (b) segmental (arrowheads); and (c) mixed (arrows show the continuous type and arrowheads show the segmental type at different levels of the cervical spine). (d) Lateral cervical radiograph shows a normal cervical spine for comparison. Bottom row: OPLL subtypes on sagittal CT multiplanar reconstruction images: (e) continuous; (f) segmental; (g) mixed; and (h) circumscribed. The ‘doublelayer’ sign (arrow) at C2 and C3 vertebral level and the ‘single-layer’ (arrowhead) sign at C4 vertebral level are seen in 6e. Note the small focal circumscribed OPLL (arrow) in 6h.
CT has greater reliability and utility in diagnosing and assessing OPLL as it provides information in three dimensions. The ossified lesions are more easily visualised on bone windows. Early OPLL manifests as multiple small bony areas within a thickened ligament, whereas mature OPLL is characterised by bony plaques with a mushroom or hill shape on axial planes. Axial CT enables assessment of the type and degree of central canal stenosis; > 60% stenosis, ≤ 6 mm of space for the cord and laterally deviated ossification pattern are associated with increased risk of developing myelopathy (
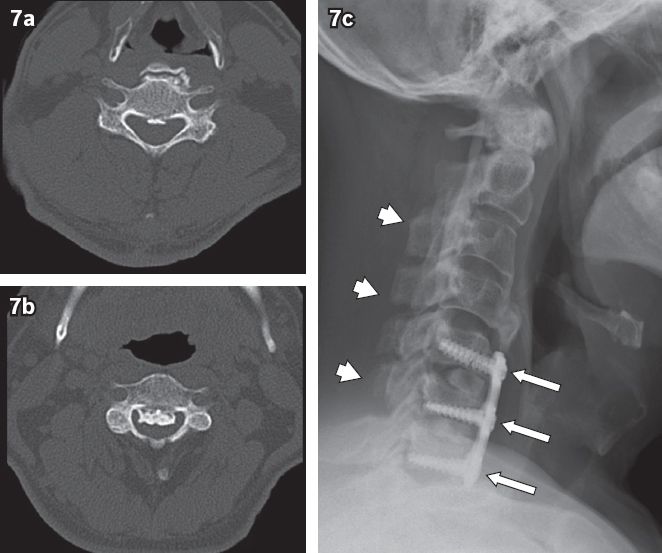
Fig. 7
Axial CT images of a patient with ossification of the posterior longitudinal ligament (OPLL) with (a) minimal central canal stenosis (at C5 level) vs. (b) severe central canal stenosis (at C3 level). (c) The patient initially underwent posterior laminoplasty (arrows) followed by anterior cervical discectomy with fusion two years later (arrowheads). The lowermost limit of the OPLL is at C4/5 intervertebral disc space.
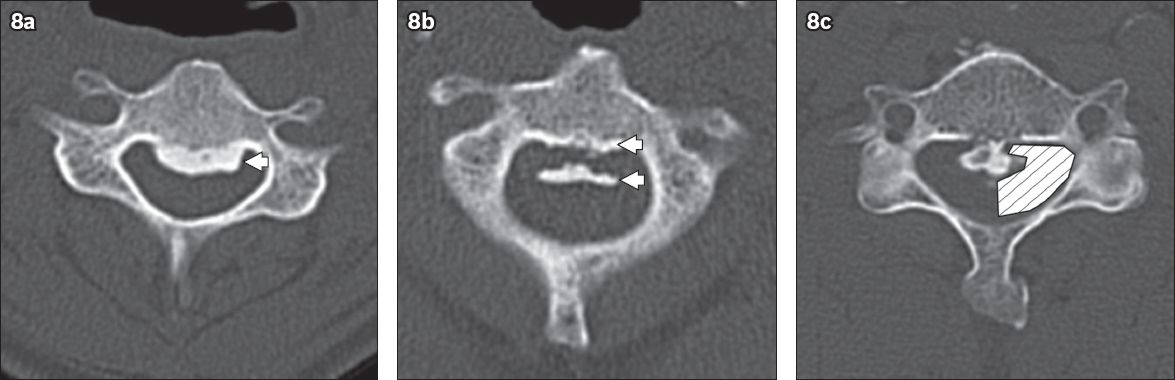
CT also allows an observer to assess for dural ossification, which is an important consideration in surgical management. When ossification involves both the PLL and the dura, it is more difficult to cleanly dissect and remove the ossified PLL from the dura during anterior decompression surgery. As such, one of the most common complications of anterior decompression surgery is cerebrospinal leak. Dural ossification is suggested by a ‘double-layer’ sign on CT (Figs.
Fig. 8
Axial CT images show (a) the ‘single-layer’ sign formed by a single ossified mass (arrowhead); (b) the ‘double-layer’ sign formed by anterior and posterior rims of ossification (arrowheads) sandwiching a central, hypodense mass; and (c) bilateral ‘C’ signs (shaded area). The ‘double-layer’ and ‘C’ signs are suggestive of additional dural ossification.
On MR imaging, the ossified lesions are hypointense on T1-weighted and T2-weighted images. This can make it more difficult to distinguish the ossified PLL from adjacent soft tissues and ligaments, in comparison to CT. However, MR imaging has great utility in the assessment of soft tissue abnormalities, such as concurrent disc protrusions and the severity of spinal cord compression. Intramedullary T2-weighted hyperintensity may indicate reversible oedema or irreversible myelomalacia, gliosis or cystic necrosis, whereas intramedullary T1-weighted hypointensity indicates irreversible necrosis and myelomalacia. Both are associated with poorer neurological outcome even after surgical decompression.(10,11) Special T2* gradient-recalled echo images can show the hypointense ossified lesions more prominently, but must be interpreted with caution, as ‘blooming’ artefact on this sequence can overestimate the extent of spinal canal stenosis.
About 70% of OPLL patients without myelopathy will remain myelopathy-free after 30 years. Therefore, prophylactic surgery is not indicated or recommended.(12) Instead, continuous observation is recommended, especially in younger patients.
Surgery should be considered in patients with progressive deficits, myelopathy or severe cord compression. The surgical approaches can be divided into anterior and posterior. Anterior decompression involves discectomy or corpectomy (in which the disc or vertebral body is removed) to expose the ossified PLL for removal or thinning. Fusion of the affected levels is then performed (
Posterior decompression involves either laminoplasty or laminectomy with fusion, and is the preferred approach when more than two or three cervical levels are affected. However, it has an increased risk of postoperative OPLL progression(13) as well as complications of C5 palsy and axial pain.(14) Laminoplasty is further contraindicated in cases of loss of cervical lumbar lordosis.
The kyphosis line (K-line) can be used to assess whether an anterior or posterior approach should be used in cervical OPLL. The K-line is drawn on CT myelography from the centre of the spinal canal at C2 level to C7 level. Loss of cervical lordosis or a large OPLL mass will contribute to extension of the OPLL beyond the K-line and thus to greater cord compression. These cases have a negative prognosis for posterior surgery.(15)
While not common, OPLL is a significant cause of myelopathy in Asians and should be considered as one of the differentials in patients presenting with myelopathy. Lateral radiographs have limitations in diagnosing OPLL and characterising disease severity; therefore, CT and MR imaging should also be performed. CT provides excellent delineation of the ossified lesions, whereas MR imaging is useful for the evaluation of associated soft tissue abnormalities. Specific radiological features on CT and MR imaging also aid in determining the likelihood of disease progression and in planning surgical management.


