Abstract
A 14-year-old girl presented with left knee pain and swelling after an injury. Magnetic resonance (MR) imaging showed a transient lateral patellar dislocation with patellar osteochondral fracture, medial patellofemoral ligament tear and underlying femoral trochlear dysplasia. Open reduction and internal fixation of the osteochondral fracture, plication of the medial patellar retinaculum and lateral release were performed. As lateral patellar dislocation is often clinically unsuspected, an understanding of its characteristic imaging features is important in making the diagnosis. Knowledge of the various predisposing factors for patellar instability may also influence the choice of surgical management. We also discuss signs of acute injury and chronic instability observed on MR imaging, and the imaging features of anatomical variants that predispose an individual to lateral patellar dislocation. Treatment options and postsurgical imaging appearances are also briefly described.
CASE PRESENTATION
A 14-year-old girl presented with pain and swelling of the left knee after accidentally twisting her knee when walking on level ground. She was subsequently unable to bear weight on her left knee. Physical examination revealed a large knee effusion and limited range of motion. What does the radiograph (
Fig. 1
Lateral radiograph of the left knee.
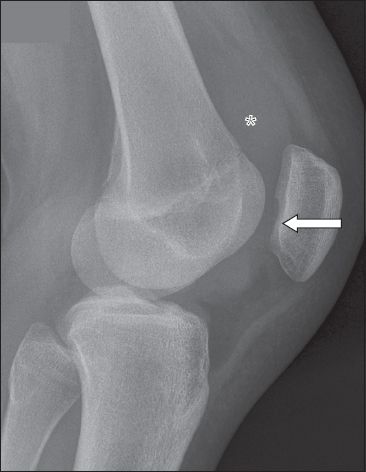
Fig. 2
(a) Sagittal fat-suppressed T2-W, (b) axial T2-W and (c) coronal fat-suppressed PD-W MR images of the left knee.
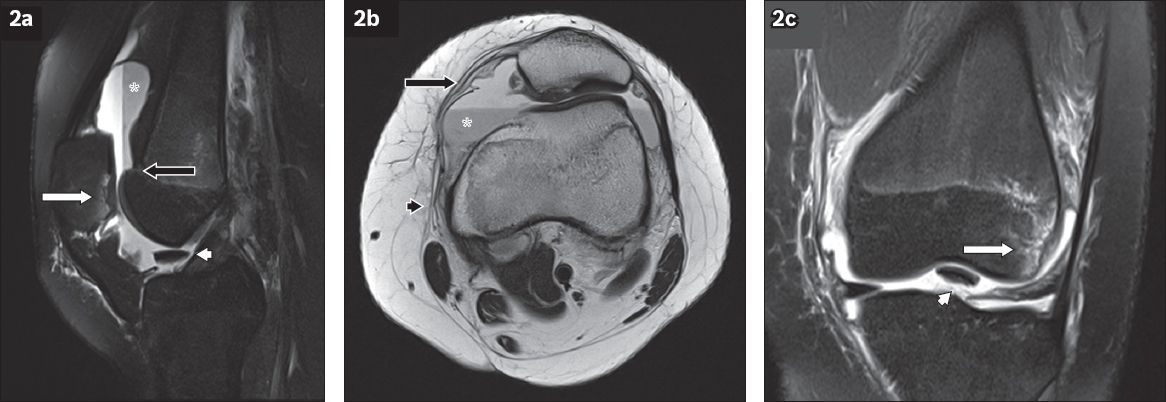
IMAGE INTERPRETATION
The radiograph shows a defect (arrow,
DIAGNOSIS
Transient lateral patellar dislocation with trochlear dysplasia.
CLINICAL COURSE
The patient underwent open reduction and internal fixation of the patellar osteochondral fracture, plication of the medial patellar retinaculum and lateral release one week after the injury. She recovered well after surgery.
DISCUSSION
The patella articulates with the femoral trochlea to form the patellofemoral joint. The patella has a tendency to dislocate laterally due to the divergent direction of pull of the quadriceps and patellar tendons (forming the Q angle, which is approximately 15º), compounded by the valgus configuration of the knee in the normal state.(1-3) Active and passive mechanisms help to stabilise the patella during knee flexion. The most important active stabiliser is the vastus medialis obliquus, the inferior portion of the vastus medialis muscle, which neutralises the action of the vastus lateralis.(3,4) Passive stabilisers include the medial ligaments (of which the medial patellar retinaculum and the MPFL are the most important) and a sufficiently deep femoral trochlea.(2,3,5,6) Anatomical variations in these areas may lead to patellar instability and a predisposition to dislocation. These variations can be accurately identified and quantified on imaging.
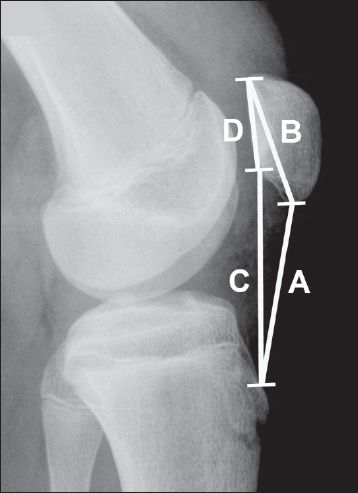
In cases of patella alta (when the patella is in a high position), there is reduced contact between the patella and trochlea during early knee flexion.(3,5,7) Using the Insall-Salvati method, patella alta is present when the length of the patellar tendon divided by the maximal diagonal length of the patella on a lateral knee radiograph produces a ratio of more than 1.2 (normal ratio: 1.0) (
Fig. 3
Lateral knee radiograph shows patella alta in a 14-year-old boy. The Insall-Salvati ratio, or the length of the patellar tendon (line A) divided by the maximal diagonal length of the patella (line B), is 1.4. In the modified Insall-Salvati method, the distance between the inferior articular surface of the patella and the patellar tendon insertion (line C) is divided by the length of the patellar articular surface (line D), giving a ratio of 2.4.
Femoral trochlear dysplasia occurs when a shallow trochlear groove reduces engagement of the patella during early knee flexion.(5) Köhlitz et al reported it as the most important contributing factor in patellar instability.(9) On true lateral radiographs, in which the posterior borders of the femoral condyles overlap or have a gap of 2 mm or less, the ‘crossing sign’ (seen in up to 96% of dysplasia cases) is present when the deepest part of the trochlear groove crosses the anterior aspect of the femoral condyles (
Fig. 4
(a) A normal lateral knee radiograph of a 19-year-old man shows that the femoral trochlear groove (black arrowheads) does not cross the femoral condyles. (b) Lateral knee radiograph of a 15-year-old boy shows the ‘crossing sign’, which occurs when the deepest part of the femoral trochlear groove (white arrowheads) crosses the anterior aspect of the femoral condyles (arrow) and is an indicator of femoral trochlear dysplasia.
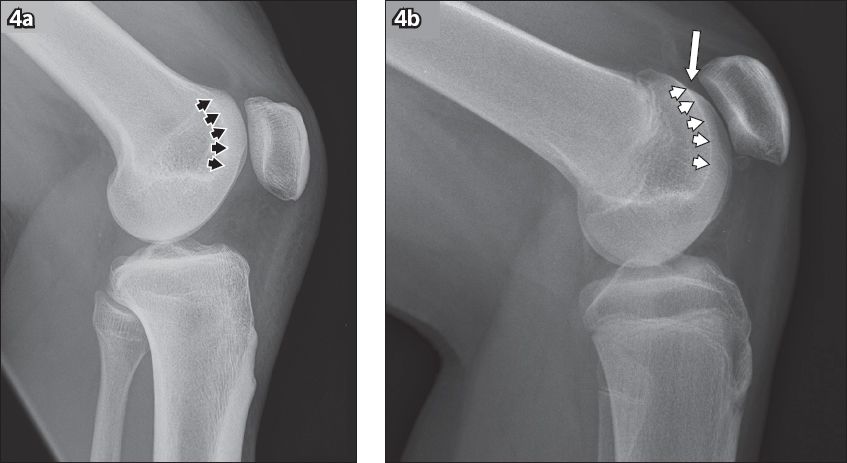
Fig. 5
Axial MR images show methods of assessing femoral trochlear dysplasia. (a) Lateral trochlear inclination in a 23-year-old man: at the apex of the intercondylar notch, the angle (dashed line) between line A, along the subchondral bone of the lateral trochlear facet, and line B, along the posterior aspects of the femoral condyles (posterior condylar axis), is 4°, indicating trochlear dysplasia. (b) Trochlear facet asymmetry in a 19-year-old woman: at 3 cm above the tibiofemoral joint cleft, the ratio of the length of the medial trochlear facet (line A) to that of the lateral trochlear facet (line B) is 0.32, indicating trochlear dysplasia. (c) Femoral depth in a 13-year-old boy: at 3 cm above the tibiofemoral joint cleft, the distance C between the deepest point of the trochlear sulcus and the posterior condylar axis (line A) is subtracted from the mean anteroposterior distance of the medial and lateral femoral condyles (lines B and D) [(B + D)/2 – C]. The femoral depth measured 3 mm in this case, indicating trochlear dysplasia.
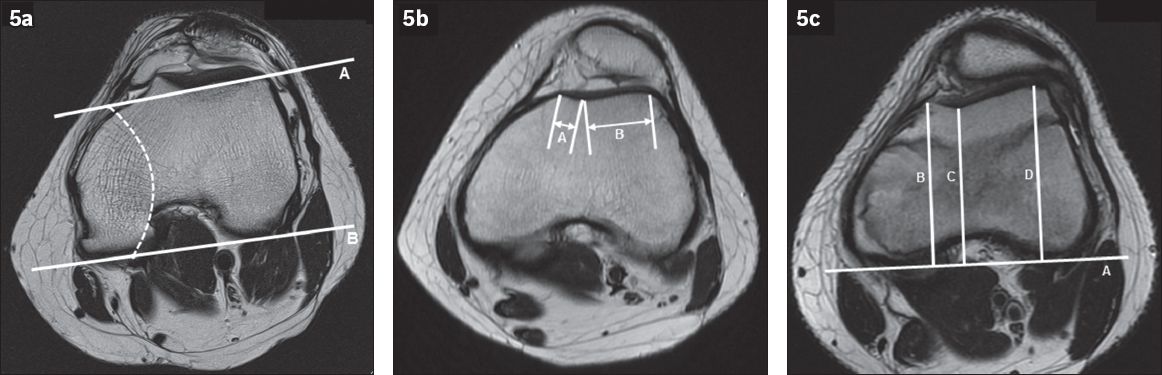
Fig. 6
Midsagittal PD-W MR image in a 23-year-old man shows a nipple-like anterior prominence (arrow) at the superior end of the femoral trochlea, which has been reported to be a highly specific sign of trochlear dysplasia.
An excessive lateral position of the tibial tuberosity can also lead to instability by increasing the lateral pull on the patella. This can be detected on CT and MR imaging by measuring the tibial tuberosity-trochlear groove (TT-TG) distance,(8) which is the horizontal distance between the deepest point of the trochlear sulcus and the tibial tuberosity on two superimposed axial images (Figs.
Fig. 7
Axial CT images of a 29-year-old man with recurrent patellar dislocation show tibial tuberosity-trochlear groove (TT-TG) distance. (a) Line B is drawn from the deepest point of the trochlear sulcus, perpendicular to the posterior condylar axis (line A). An axial image of the tibial tuberosity (b) is superimposed on the first image to form image (c). Line C is drawn from the tibial tuberosity, perpendicular to line A. The distance between lines B and C (TT-TG distance, double-headed arrow) is measured (25 mm in this case).

Lateral patellar dislocation, which most commonly affects adolescent females, usually occurs when the aforementioned predisposing factors are present.(1,5,12) It most often results from a twisting injury with knee flexion, as the femur rotates internally on a fixed tibia.(1,5,13) As the patella frequently relocates spontaneously, the diagnosis may be clinically unsuspected or misdiagnosed in up to 73% of patients; hence, imaging plays a very important role in diagnosis.(1,2,6)
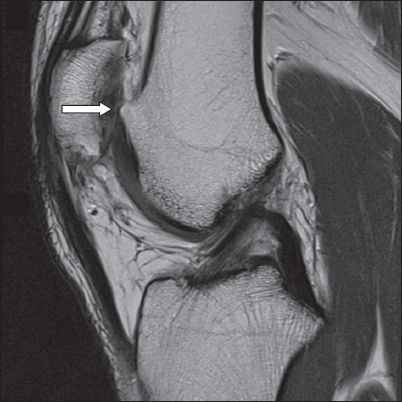
Characteristic patterns of osseous injury are seen on MR imaging. As the patella relocates, the inferomedial patella impacts upon the anterolateral aspect of the lateral femoral condyle, leading to bone contusions. These are visualised as focal areas of high T2-weighted and low T1-weighted signal intensity (i.e. the classic ‘kissing’ contusion pattern) (white arrows in Figs.
Fig. 8
Axial fat-suppressed T2-W MR image in a 15-year-old boy shows the characteristic ‘kissing’ bone contusions at the inferomedial patella (white arrow) and lateral femoral condyle (black arrow). Note also the avulsion of the medial patellofemoral ligament from its femoral attachment (arrowhead).
The MPFL and medial retinaculum may be injured in up to 70%–100% of patients.(1,5) The MPFL is normally seen on axial and sagittal T2-weighted sequences as a well-defined, low-signal-intensity band extending from between the adductor tubercle and the medial femoral epicondyle towards the medial patella (
Fig. 9
Axial T2-W MR images of three patients. (a) Normal medial patellofemoral ligament (MPFL) in a 19-year-old man: a well-defined, low-signal-intensity band (arrow) extends from between the adductor tubercle and the medial femoral epicondyle towards the medial patella. (b) Complete MPFL tear in a 22-year-old man: the MPFL (arrow) shows complete discontinuity of its fibres near its femoral attachment (arrowhead), with extensive surrounding oedema. (c) Partial MPFL tear in an 18-year-old woman: the MPFL (arrow) shows thickening and irregularity of its fibres at its femoral attachment (arrowhead), with intrasubstance and surrounding oedema.

Fig. 10
Coronal fat-suppressed PD-W MR image in a 22-year-old man shows oedema (arrow) around the inferior portion of the vastus medialis obliquus muscle.

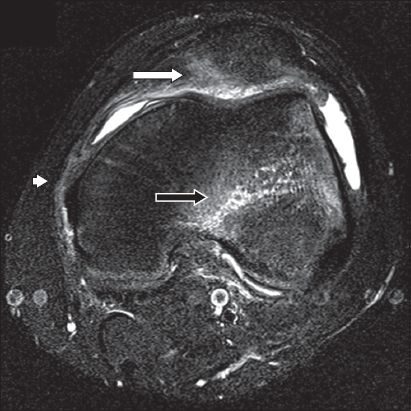
A joint effusion is often seen if imaging is performed early.(1) There may be a fluid-fluid level in a haemarthrosis due to sedimentation of blood components (*, Figs.
Patellar instability is also associated with oedema in the superolateral portion of Hoffa’s (infrapatellar) fat pad.(2,8,15) This may be due to impingement of fat between the patellar tendon or lateral patellar facet and the lateral femoral condyle.(15) The oedema is best seen as high signal on the far lateral sagittal images of a fluid-sensitive sequence (
Fig. 11
(a) Coronal fat-suppressed PD-W and (b) sagittal fat-suppressed T2-W MR images in a 23-year-old man show oedema in the superolateral portion of Hoffa’s (infrapatellar) fat pad (arrows), in keeping with impingement.
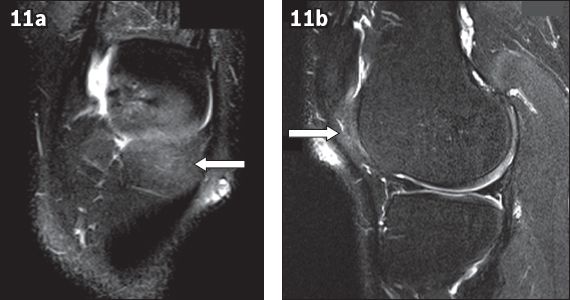
Fig. 12
Axial CT image in a 20-year-old man shows ligamentous ossification of the medial patella (arrow).

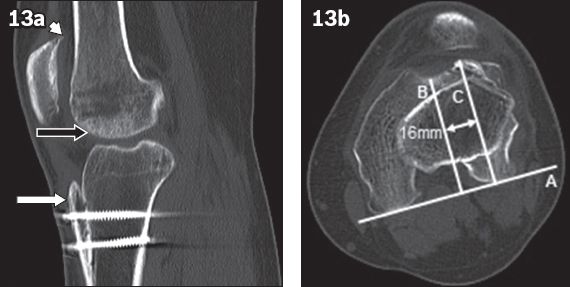
Fig. 13
(a) Sagittal CT image post-tibial tuberosity transfer in a 29-year-old man (patient in
First-time patellar dislocations are usually managed conservatively with rest, ice, compression, elevation (RICE) and immobilisation with a brace in extension for 3–6 weeks.(1,3,5) Physical therapy consisting of quadriceps strengthening (focusing on the vastus medialis obliquus) and hamstring stretching is also performed.(1,3) Indications for surgery in the acute setting include the presence of osteochondral fragments or loose bodies, which require surgical reattachment or resection, and femoral avulsion of the medial stabilisers, which may require surgery to fully restore the patella to its normal position.(1,5) Surgery is also indicated in recurrent patellar instability, which may occur in up to 50% of cases managed conservatively.(3,5,7,12) The choice of surgical procedure depends on the underlying anatomical anomaly and its severity. The most common surgical procedure performed is a combination of medial capsular plication, which involves suturing the tear in the medial stabilisers, and release of the lateral patellar retinaculum.(5) This can often be performed arthroscopically.(5) Reconstruction of the MPFL with an autograft (e.g. gracilis tendon) or an allograft (e.g. semimembranosus tendon) is increasingly performed in lieu of medial plication.(1,5,7) In patients with a TT-TG distance of more than 20 mm, transfer of the tibial tuberosity to a more medial position can be performed to reduce the lateral force on the patella (
As lateral patellar dislocation is often clinically unsuspected, an understanding of its characteristic imaging features (particularly on MR imaging) is important in making the diagnosis. Imaging also allows for accurate identification of potential sites of injury and anatomical variants that predispose an individual to lateral patellar dislocation, which may affect the timing and choice of surgical management.


